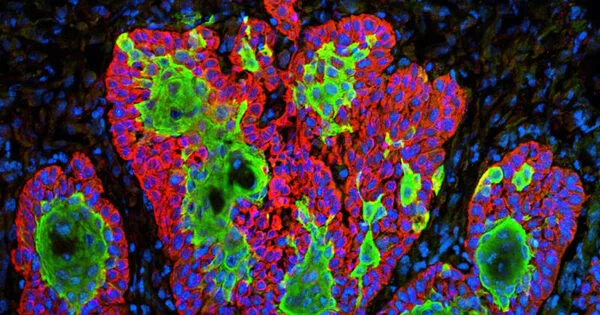
A visualization technique that combines high-speed cameras and fluorescent injection to identify tumor tissue from normal tissue across cancer kinds has been developed by researchers. The scientists tested the novel imaging technology, known as fluorescent lifetime imaging (FLT), on tissues from more than 60 cancer patients who had surgery. The approach was claimed to be over 97 percent accurate across tumor types, with the potential to improve cancer surgery accuracy.
Removing a tumor while preserving good tissue demands extreme precision, but surgeons must frequently rely on their eyes and hands to identify where to cut. A team lead by Mass General Brigham researchers developed a visualization tool that uses high-speed cameras and fluorescent injection to identify tumor tissue from normal tissue across cancer types.
The scientists tested the novel imaging technology, known as fluorescent lifetime imaging (FLT), on tissues from more than 60 cancer patients who had surgery. The team stated that the technique was over 97 percent accurate across tumor types in a publication published in Nature Biomedical Engineering, with the potential to increase the accuracy of cancer procedures.
Our lab has been studying fluorescence lifetime imaging since 2002, but no one has combined it with tumor imaging and injectable dyes in humans. We’ve created a technique for accurately identifying tumor tissue from healthy tissue across cancer types by doing so.
Anand Kumar
“This collaboration has been thrilling,” said corresponding author Anand Kumar, PhD, of Massachusetts General Hospital’s Athinoula A. Martinos Center for Biomedical Imaging. “Our lab has been studying fluorescence lifetime imaging since 2002, but no one has combined it with tumor imaging and injectable dyes in humans. We’ve created a technique for accurately identifying tumor tissue from healthy tissue across cancer types by doing so.”
Kumar collaborated closely with colleagues at Mass Eye and Ear, which is part of the Mass General Brigham healthcare system and treats patients with head and neck cancer.
“We are on the verge of a revolution in solid tumor surgery,” said Mark Varvares, MD, chief of Otolaryngology-Head and Neck Surgery at Mass Eye and Ear. “By using the advanced imaging techniques combined with the dye, surgeons in the near future will have the ability to more completely remove all malignant cells during tumor surgery while at the same time, with confidence, spare normal tissue, enhancing postoperative function and in some cases, the patient’s appearance.”
Mass General Brigham has 16 member facilities, including academic medical centers, top-tier specialty hospitals, community hospitals, a rehabilitation network, and more. Research that spans more than one of these entities is more than the sum of its parts, helping to provide insights and unique perspectives from multiple settings and areas of expertise.
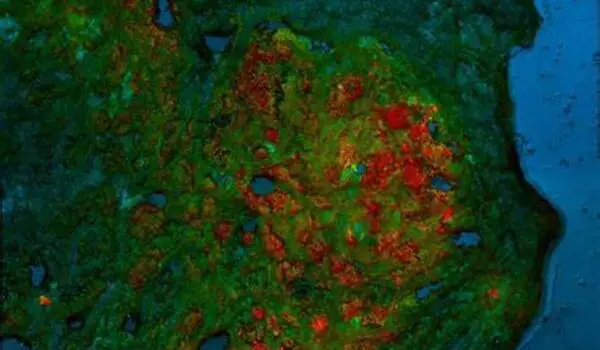
Many technologies have been pursued to improve visualization of tumors during surgery, including fluorescence imaging and advanced microscopy, but such technologies have not yet been widely adopted and most are restricted to specific types or subtypes of cancer. Fluorescence imaging can use dyes to target cancer-specific molecules, but standard imaging techniques can have limited accuracy for detecting tumor margins — or the edges of normal tissue that surround a tumor — since the expression of these molecules can vary widely within and across tumor types.
Kumar and colleagues’ technique, known as FLT imaging, takes a different approach. Rather than depending solely on dyes to target cancer, the technology use high-speed cameras to detect changes in the properties of light emitted by tissue. In prior preclinical experiments, Kumar and colleagues discovered that tumors in mice injected with the dye indocyanine green (ICG) exhibited a longer fluorescence lifetime than normal tissue. This distinction enabled the researchers to discriminate between tumor and normal tissue.
In their latest work, the researchers used the same concept using patient samples. The researchers began by evaluating samples from MGH patients undergoing liver surgery and Mass Eye and Ear patients undergoing head and neck surgery. Patients had received an ICG injection at least a day before the surgery.
Building on this preliminary work, the team collaborated across institutions to evaluate specimens from more than 60 patients with cancers ranging from the liver to the brain, tongue, skin, bone, and soft tissue who were treated at MGH, Mass Eye and Ear, The University of Pennsylvania, the University of Newcastle in the United Kingdom, and Leiden University in the Netherlands. The researchers discovered a FLT shift at the cellular level that was constant across tumor types and patients. The technology could also tell the difference between benign and metastatic lymph nodes. It was more than 97 percent accurate in differentiating tumor tissue from healthy tissue in general.
The authors point out that, while ICG is approved by the FDA for various uses, it is not yet licensed for clinical use as a tumor marking agent. The next step for the researchers is to conduct a larger-scale clinical trial to evaluate the safety and efficacy of fluorescent lifetime imaging with ICG for tumor identification during surgery.
“Our work suggests that the combination of fluorescence lifetime imaging with ICG could improve surgical resections, thereby impacting patient lives,” Kumar pointed out. “We’re excited to take these next steps to move our discoveries closer to clinical impact.”