Introduction
The impacts of HIV/AIDS on a country are tremendous. AIDS kills millions of people, thus weakening the workforce, fracturing and improvising families, and leaving millions of children orphaned, with concomitant effects on the whole political, social and economic fabric of a country.
Bangladesh is still considered as a low HIV/AIDS prevalent country. However, it is at a critical moment in the course of its AIDS epidemic. It is estimated that there are 13,000 HIV-positive people in the country and that HIV prevalence in the adult population is less than 0.01%. However, the country’s vulnerability is very high. National HIV surveillance indicates that the rate of HIV infection among street-based sex workers in central Bangladesh is high compared with sex workers in other parts of South Asia. HIV among injecting drug users is already 4%.
The presence of covert multi-partner sexual activity and denial, the low level of knowledge and low condom use, unsafe professional blood donations, lack of a desirable environment and violation of Human Rights, all contribute to the spread of HIV in Bangladesh.
The awareness of HIV/AIDS in the Bangladeshi population remains quite low. One recent survey found that “Only 19 percent of ever-married women and 33 percent of currently married men had heard of AIDS.” As a low HIV prevalent country, that has interventions for highly vulnerable populations supported by other agencies, WHO considers creating awareness on HIV/AIDS as a priority intervention at school level. Family life education in Bangladesh is still at its infancy. As a first step the WHO is supporting the National STD/AIDS Programme to orientate teachers on HIV/AIDS. A series of programmes started through out the country with the first workshop being held in the office of the Sirajgong Civil Surgeon in August 2003 with an encouraging 90% female teacher participation.
Blood safety is one of the priority issues for prevention of HIV/AIDS, especially in Bangladesh as professional donors are still one of the significant groups of donors. There is also evidence that many drug users are also professional blood donors. WHO in Bangladesh supports the training of doctors on blood safety. In addition to transfusion medicine related issues such as the screening of Transfusion Transmitted Infections, the programme emphasises the need to reduce unnecessary transfusions through the appropriate clinical use of blood including the use of intravenous replacement fluids and other simple alternatives to transfusion, wherever possible. WHO is also working on the detailed work plan related to blood safety which the Ministry of Health and Family Welfare is proposing to implement using credit it has received from the World Bank.
South-East Asia Region has one of the fastest growing AIDS epidemic in the world. Since HIV made its entry into the region in the 1980s, every country has seen new infections. As of April 2001, it is estimated that India with 3 860 000 has the highest number of HIV infected adults and Thailand the highest number AIDS with 156 309 reported cases in the South-East Asia Region. High-risk behaviors’ and vulnerability that promote HIV transmission are present in all countries and therefore, there is no room for complacency for those countries who presently have low prevalence. This being the current scenario, it is imperative to consider the role and responsibilities of all health care providers and particularly nursing and midwifery. By virtue of numbers and close and continuous contact with individuals, families and communities, nurses and midwives have huge potential for development.
Bangladesh is still considered as a low HIV/AIDS prevalent country. However, it is at a critical moment in the course of its AIDS epidemic. It is estimated that there are 13,000 HIV-positive people in the country and that HIV prevalence in the adult population is less than 0.01 percent. However, the country’s vulnerability is very high. National HIV surveillance indicates that the rate of HIV infection among street-based sex workers in central Bangladesh is high compared with sex workers in other parts of South Asia. HIV among injecting drug users is already four percent.
Rationale of the study
Bangladesh is still considered as a low HIV/AIDS prevalent country. However, it is at a critical moment in the course of its AIDS epidemic. It is estimated that there are 13,000 HIV-positive people in the country and that HIV prevalence in the adult population is less than 0.01 percent. However, the country’s vulnerability is very high. National HIV surveillance indicates that the rate of HIV infection among street-based sex workers in central Bangladesh is high compared with sex workers in other parts of South Asia.
In recent years, knowledge about HIV and AIDS has increased across the country. Most adolescents were aware of HIV/AIDS. Study findings suggest that ninety-three percent of the male and 78 percent of the female adolescents either knew about or had heard of HIV. Similarly, a large number of the adolescents had knowledge on routes of HIV transmission. Most (90 percent) adolescents could correctly mention that the major routes of HIV transmission are: receiving HIV-infected blood transfusion, using non-sterilized syringe, having unsafe sex, and having sex with multiple sexual partners. However, the adolescents had some misconceptions about the routes of HIV transmission. Although the knowledge of transmission is high but still a significant percentage (15 percent) of adolescent did not know how to prevent it. It was also found that the proportion having knowledge on the prevention of HIV/AIDS was almost equal between the male and the female adolescents, except the use of condom during sex. It is critical to improve the knowledge of spread as well as prevention of HIV among the all age group. Thus a cross sectional study will be undertaken among the patients who will seek treatment from infections Disease Hospital, Comilla. It is expected that the study findings will help to formulate plan strategy for enhancing knowledge of patients about HIV/AIDS in Bangladesh.
Literature Review
Age segregated data shows that HIV and AIDS are common among the people who are 16 to 45 years. About one-fifth of the HIV and AIDS infected people are within 16 to 25 years of age. Though 77 percent of the HIV infected/positives are married but still a significant percentage of HIV and AIDS positive or infected are unmarried adolescents and youth (13.2 percent).
In recent years, knowledge about HIV and AIDS has increased across the country. Most adolescents were aware of HIV/AIDS. Study findings suggest that ninety-three percent of the male and 78 percent of the female adolescents either knew about or had heard of HIV. Similarly, a large number of the adolescents had knowledge on routes of HIV transmission. Most (90 percent) adolescents could correctly mention that the major routes of HIV transmission are: receiving HIV-infected blood transfusion, using non-sterilized syringe, having unsafe sex, and having sex with multiple sexual partners. However, the adolescents had some misconceptions about the routes of HIV transmission. Although the knowledge of transmission is high but still a significant percentage (15 percent) of adolescent did not know how to prevent it. It was also found that the proportion having knowledge on the prevention of HIV/AIDS was almost equal between the male and the female adolescents, except the use of condom during sex.
Literature review suggests that there is lack of knowledge among the adolescents about STIs in Bangladesh (NIPORT, Mitra and Associates, and Macro International 2009; NASP 2009; Hena 2009; Rob 2005; Wasserheit 1989). Study findings also show that only 25 percent of the male and five percent of the female adolescents were aware of STIs, except HIV. Half of the male and a little over one-fourth of the female adolescents mentioned avoiding sex with an STI-infected person as a way of preventing STIs. About a similar proportion of the male and female adolescents mentioned use of condom during sex as a preventive measure. The rural male adolescents were more likely to have knowledge about the ways of preventing STIs than their urban counterparts. Findings suggest that 22 percent unmarried male are sexually active and it was common among out of school male (NASP 2009). In Bangladesh, formal SRH education and health services for adolescent and youth are limited especially for unmarried people (NASP 2009). The Bangladesh Demographic and Health Survey (BDHS), 2004 showed that about a four-fifth of currently married men did not have any knowledge of STIs and only one-tenth knew about two or more symptoms of STIs.
Although young Bangladeshis are at risk of HIV very few believe so – 22 percent of unmarried males reported having premarital sex, almost 60 percent of whom had never used condoms. This has impacted on the rate of STIs; almost one in five men, and two in five adolescent boys, reported having at least one symptom of a sexually transmitted infection (STI) in a 2004 health survey. Women also require special attention in HIV interventions in Bangladesh, given their social, economic and political status. Women are four times more likely to contract HIV than men. Women’s lower social and cultural status also causes them to have less access to education, employment opportunities and health care, including opportunities for HIV tests, counseling and medical care. Women are often subjected to early marriage, sexual abuse and violence in intimate and marital relationships. An increasing number of women are forced to sell their bodies as the only way to survive and provide for their children. Men who buy sex from women are often reluctant to use condoms. As one man said: “Why should I use a condom when I am paying to get pleasure?” Because women have little negotiating power, even within their marriages, they may have unprotected sex with their spouses who might be engaging in one or more high-risk behaviors and be exposed to HIV. The HIV prevalence among the general public is not fully known; currently available surveillance data only covers high risk groups. This ambiguity is partly because voluntary and confidential counseling and testing (VCT) services are not widely available in Bangladesh. While HIV tests are available in some private health settings, in many cases there is no counseling support and no confidentiality guarantee. Many HIV positive people tested both in private and government facilities have seen their names and other personal details published in the local or national media. Social values, lack of adequate information, the stigma attached to HIV and AIDS, and the lack of confidentiality are not conducive for people, especially the younger population, to seek out HIV tests (http://www.unicef.org/bangladesh/HIV_AIDS(1).pdf, HIV and AIDS in Bangladesh).
Mukta Sharmaa 2009 An estimated 800000 PWID live in the WHO South- East Asia Region. HIV prevalence among PWID in countries of the South-East Asia Region varied widely (0% in the Maldives to 52% in Indonesia). Bangladesh, currently, has a elatively lowHIV prevalence of 7.1% but is showing a rising trend. In many cities, HIV prevalence among PWID has remained above 25% over the past 5 years. Analyses of country-wise trends show that HIV prevalence has been high and stagnant in Thailand, Myanmar and most states of India and is rising in Indonesia and Bangladesh. Exceptionally, in Nepal, HIV prevalence has decreased in all the regions. Little information is available on HIV incidence in populations of PWID. Recent modelling data from Thailand suggest that HIV incidence is the highest among PWID (2.6 per 100 per year). In parts of the northeastern states of India (Manipur and Nagaland), HIV incidence as measured by prevalence among young PWID (aged 15–24 years) has decreased from 11% in 2003 to 3.2% in 2007 [32]. National sentinel surveillance data indicated a wide variation in the reported HIV prevalence within countries. In India, HIV prevalence was highest (typically over 15%) in the metropolitan cities, Punjab, and the North-East but below 5% in states such as Karnataka, Andhra Pradesh, Uttar Pradesh and Bihar. In Myanmar, HIV prevalence among PWID ranged from 19% in Yangon to 54.5% in Myitkyina.
Bangladesh and India reported the highest rates of needle–syringe sharing [data from behavioral sentinel surveys (BSS)]. Routine BSS data were not available for Thailand; however, one study reported that 80% of its participants had occasionally shared injecting equipment in the past 12 months. Rates of unsafe injecting and sexual risk behaviors were also high. Exceptionally, despite high levels of syringe sharing in Bangladesh, HIV prevalence among PWID is comparatively low, though it has grown five-fold from 1.7 to 7.1% in the capital Comilla. Postulated reasons include limited sexual transmission among PWID (and to their sexual partners) due to the high prevalence of male circumcision and declining syphilis rates, small size of sharing networks and patterns of drug use that limit HIV transmission. Notably, harm reduction interventions including large-scale NSPs began in 1998 when HIV prevalence among PWID was still below 1%, and modeling data suggest that this may have reduced HIV incidence in Comilla by over 90%. A reduction in needle–syringe-sharing behavior was evident in Nepal. In Kathmandu, rates of needle–syringe sharing had declined from 45% in 2002 to 12% in 2007. Concomitant declines were noted in HIV prevalence among PWID, from nearly 70% in 2002 to 34% in 2007. Rates of sharing equipment at last injection declined from 55% in 2001 to 26% in 2006 in north-east India (Manipur), and HIV prevalence declined from nearly 52% in 2002 to just over 13% in 2007. Other risk behaviors In Bangladesh, the proportion of PWID who bought sex in the last year from a female sex worker varied from 46 to 66%, whereas consistent condom use in the past year ranged from 14 to 43%. During the last sexual encounter with a sex worker, less than 35% of male PWID reported condom use in Indonesia and just over 37% in Nepal. Vulnerability to HIV among PWID is enhanced by high rates of sexually transmitted infections (STIs). Integrated behavioral and biological assessments (IBBAs) conducted in Nagaland (India) showed active syphilis rates o 7–20% in 2008 [45]. Syphilis rates among female injectors are also high; in one site in Bangladesh, 10% were infected in 2006–2007. Magnitude of and trends in HIV infection among incarcerated people who inject drugs Data in this area are scarce. HIV prevalence among prisoners in India, Indonesia and Thailand is generally above 10%. HIV transmission in prisons may be fuelled by risk behaviors such as sharing of injecting equipment.
A study among 95 inmates in five prisons in eastern Nepal found that 28% used drugs and, of these, 75% ‘always’ shared needles. In a prospective cohort of 705 PWID in Klong Prem Prison in Thailand, 38% had injected while in prison, and 97% of these had shared injecting equipment. Behavioural surveys in the Maldives also indicated that 32% of PWID had injected while in prison. In Jakarta, Indonesia, routine sentinel surveillance data show HIV prevalence in prisoners of more than 10% in four sites. A sampling of all prisoners in 2003 showed that only 5–10% was HIV positive on entry to prisons, but approximately 20% of the total population was infected, suggesting that HIV is transmitted in prisons through risk behaviors. In Timur Cipinang Prison in Jakarta, HIV prevalence increased from 17.8% in 2005 to 30.4% in 2006. Similar data among incarcerated PWID are not available from other countries of the region. Availability and reach of harm reduction interventions in countries Needle–syringe programmes The number of NSP sites ranged from 159 in Indonesia to none in the Maldives (personal communication, National AIDS Programme Managers). Bangladesh reported the highest ratio of NSP-to-PWID populations (based on midpoint of population estimate) – one NSP for every 333 PWID (90 divided by 30 000). Myanmar has only one NSP per 3900 PWID (19 divided by 75 000). In Nepal, India and Indonesia, one NSP was available for 869, 1239 and 1378 PWID, respectively. NSPs are not officially available in Thailand or the Maldives, though there are anecdotal reports of small-scale informal syringe distribution. The reach of NSPs is the highest in Bangladesh – between 31 and 61% of the lower and upper national size estimates of PWID in 2006. In 2008, it was between 44 and 88%, with 17 582 PWID accessing NSPs in the past 12 months (NAP, Bangladesh, personal communication). The National AIDS Commission in Indonesia reported 22% coverage with NSPs in 2007, with over 49 000 of the estimated 219 000 PWID accessing services during the year. In Myanmar, 29 411 of the estimated 75 000 PWID (28%) were reached with HIV prevention services in 2007. The NAP in Nepal indicated that, in 2007, 31% of PWID were reached with NSPs. Data on the frequency/regularity of contact with services were not available. The actual numbers of needles and syringes distributed from NSPs in comparison with the estimated need were low – in Nepal, 988 000 needles and syringes were distributed in 2006 – as opposed to an estimated need of 21 000 000. This indicates that the national AIDS programme provides less than 5% of the required needles and syringes in Nepal. In Myanmar, 2 091 166 needles and syringes were distributed in 2007 as opposed to an annual requirement of at least 27 million. No data are available on the number of needles and syringes bought by individuals through pharmacy outlets.
Millions of people worldwide are injecting drug users (IDUs), and blood transfer through the sharing of drug taking equipment, particularly infected needles, is an extremely effective way of transmitting HIV. Around 30% of global HIV infections outside of sub-Saharan Africa are caused by the use of injecting drugs, and it accounts for an ever growing proportion of those living with the virus.1
The illegal nature of injection drug use can also create barriers to accessing adequate treatment and prevention services making IDUs more vulnerable to HIV and its effects. The crossover with prostitution further means they are in positions to transmit the virus between other at-risk populations.
Universal Precaution Practice:
Judging from the responses of the national nursing focal persons, focus group discussions with nurse educators and observation from the hospitals visited, it appears that universal precaution policy is not being implemented in all the hospitals of many countries in the Region. Bhutan, Myanmar and Thailand report universal precaution as being implemented in all hospitals within the country.
Findings from the KAP survey, focus group discussions with nurse educators and hospital staff and few nursing superintendents are as follows:
• 228 nurses (82%) of the 276 respondents of the KAP questionnaire reported following universal precaution guidelines strictly.
• 42 nurses (15%) said they could not follow all the precautions due to shortage of supplies. It is surprising only 15% reported shortage of supplies since this issue was a pointed out as a concern by the staff of many hospitals visited. In Myanmar, the wards have a system of ward fund raising through donations from well-to-do patients. Money thus collected is used to buy gloves and disinfectants when government supplies run out. An auxiliary nurse midwife in a rural health post in Rajasthan, India has no supplies of gloves or disinfectants. She buys disposable plastic gloves and disinfectants using her own money.
• Four nurses (1.4%) said they avoided risky procedures that could expose them to HIV.
• In Thailand, nurses are designated as infection control nurses. They take responsibility for monitoring and supervision of infection control activities. This is not being practised in many hospitals of the other member countries.
• Several hospitals and nursing schools commented that nursing staff should be protected with hepatitis vaccination, while some hospitals have already implemented this.
• Sweepers and cleaners who are the ones who usually clean up blood spills and other wastes, do not normally receive any formal training on Universal Precaution.
Knowledge, Attitude and Practice of Practicing Nurses/Midwives on HIV/AIDS:
With regard to basic knowledge of HIV/AIDS, 220 nurses (79%) could tell the commonest mode of HIV transmission and 146 (53%) could describe window period correctly. 204 nurses (74%) knew the full form of HIV. Less than half, 115 nurses (42%) were able to identify the best method of prevention (maybe the question was poorly framed). Less than half, 134 nurses, (48%) could tell the common major signs that help in provisional diagnosis of AIDS. As opposed to 186 nurses (67%) only 58 nurses (21%) have heard of cases of nurses refusing to provide nursing care to PLHA, however 21% is still a large percentage of nurses, considering nurses are the main care providers while PLHA are in hospitals.
While 120 nurses (43.5%) said AIDS patients should be nursed in isolation to protect the patient from infections, 52 nurses (18.8%) felt AIDS patients should be nursed in isolation to protect others from being infected with HIV. 220 nurses (79.7%) said identity of an HIV positive patient should be revealed to protect nursing staff from infection. Although a large majority of nurses claimed to follow universal precaution practices strictly, obviously the principles are not well understood by many nurses. While 33 nurses (12%) said they were extremely afraid of being in contact with AIDS patients, 118 (42.8%) said they were a little afraid. Overall, more than half the respondents (54.7%) admitted to being afraid. 125 (45%) said they were not afraid at all. Of the 276 respondents, 30 nurses (11%) reported having had no experience of caring for PLHA. With regard to the practice of universal precaution, 228 (82.6%) of nurses reported following universal precaution practices strictly and 42 (15.2%) said they could not follow all practices due to shortage of supplies. Four nurses (1.5%) said they avoided risky procedures that may expose them to HIV infection.
Research Question
What is the current status of knowledge on HIV and AIDS among patients who will seek treatment from Infectious Disease Hospital (IDH)?
Research Objective
General Objective
To assess the knowledge of HIV and AIDS among patients who will seek treatment from Infectious Disease Hospital (IDH).
Specific Objectives
- To explore the knowledge on signs and symptoms of RTIs, STIs and HIV/AIDS and the ways of transmission and prevention among the respondents.
- To assess the source of knowledge of HIV/AIDS to the respondents
- To collect the recommendation from the respondents on how to improve the respondent’s knowledge on HIV/AIDS.
- To know the socio demographic characteristics of the respondents.
Operational Definition
RTIs: Reproductive tract infection (RTIs) are infections that affect the reproductive tract, which is part of the Reproductive System. For females, reproductive tract infections can be in either the upper reproductive tract (fallopian tubes, ovary and uterus), and the lower reproductive tract (vagina, cervix and vulva); for males these infections are at the penis, testicles, urethra or the sperm tube.
STIs: It is an illness that has a significant probability of transmission between humans or animals by means of sexual contact, including vaginal intercourse, oral sex, and anal sex. While in the past, these illnesses have mostly been referred to as STDs or VD, in recent years the term sexually transmitted infection (STI) has been preferred, as it has a broader range of meaning; a person may be infected, and may potentially infect others, without showing signs of disease.
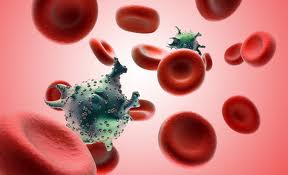
HIV: Human immunodeficiency virus (HIV) is a lentivirus (a member of the retrovirus family) that causes acquired immunodeficiency syndrome (AIDS), a condition in humans in which the immune system begins to fail, leading to life-threatening opportunistic infections. Infection with HIV occurs by the transfer of blood, semen, vaginal fluid, pre-ejaculate, or breast milk. Within these bodily fluids, HIV is present as both free virus particles and virus within infected immune cells.
AIDS: Acquired immune deficiency syndrome or acquired immunodeficiency syndrome (AIDS) is a disease of the human immune system caused by the human immunodeficiency virus. This condition progressively reduces the effectiveness of the immune system and leaves individuals susceptible to opportunistic infections and tumors.
Knowledge Scale:
- Know what is HIV/AIDS?
- Know the sign symptoms of HIV/AIDS.
- Know the route of transmission.
- Know how infection spread.
- Know vulnerable groups.
- Know about high risk factors.
- Know how to prevent.
- Know about STD.
- Know the SS of STD.
- How to prevent from STD.
Very good knowledge: When answer was found corrected for 8 to 10 questions then it was scored as very good knowledge.
Good knowledge: When answer was found corrected for 5 to 8 questions then it was scored as good knowledge.
Satisfactory knowledge: When answer was found corrected for 3 to 5 questions then it was scored as satisfactory knowledge.
Poor knowledge: When answer was found corrected for below 3 questions then it was scored as poor knowledge.
Key variables
Dependent Variables
Knowledge level of patients on HIV/AIDS
Independent variables
- Age
- Sex
- Residence
- Religion
- Monthly income
- Education
- Occupation
- Knowledge about the sources and possible prevention of HIV AIDS
Type of Study
A cross sectional hospital based descriptive study will be conducted in Infectious Disease Hospital (IDH), Comilla.
Study place
Infectious Disease Hospital (IDH), Comilla.
Study population
Patients will seek treatment from Infectious Disease Hospital (IDH), Mohakhali, Comilla will be selected for the study.
Inclusion criteria
- Male or female who will seek treatment from the Infectious Disease Hospital (IDH), Mohakhali, Comilla.
- Age 15-45.
Exclusion Criteria
- Not willing to participate in the study.
Sample Size
The sample size will be 100 patients will be selected purposively.
Sampling formula
The sample size was calculated on basis of the following formula:
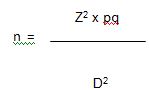
Where,
N = Sample size estimate
Z = Z for level of significance alpha (at 0.05 level of significance value of Z is 1.96)
p= 30%
q= 1-p
d= acceptable margin of error (.05)
Actual sample size was
(n) = Z² pq/d²
= (1.96) ² × 0.3 × 0.3/ (0.05) ²
= 100
Sampling Technique
Non probable purposive sampling technique.
Data Collection Tools
For smooth conduction of the study, a structured questionnaire will be developed. The questionnaire will have several parts. The first was on respondent’s socio demographic information’s, second part on their knowledge on HIV and AIDS and other STD/STIs.
Data Collection Procedure
After explaining the purpose of the study data will be collected through face to face interview using Bengali structured questionnaire.
Conduction of the study, quality control and monitoring
The investigator herself will be collected data from selected hospital. The collected data will be checked and verified by the investigator at the end of the work every day. Any inaccuracy and inconsistency will be corrected in the next working day. However, cross checking of the collected data will be made randomly.
Data Processing and data analysis
The data entry will be started immediately after the completion of data collection. The collected data will be checked, verified and then entered into the computer. Only fully completed datasheet will be entered into the computer for the final analysis. The analysis will be carried out with the help of SPSS (Statistical Package for Social Science) Windows software program.
Ethical consideration
Before to the commencement of this study, the research protocol will be approved by the research committee of ADUST. The aims and objectives of the study along with its procedure, risks and benefits of this study was explained to the respondents in easily understandable local language and then informed consent will be taken from each participant. Then it was assured that all information and records will be kept confidential and the procedure will be used only for research purpose.
Informed Consent
A well and clearly understood inform consent form will be filled in up by the respondents and interviewer. This ensured that each of participants got the information they need to make an informed decision.
Results
Figure : Distribution of the respondents by sex
Out of the 100 repondents, 66 of them were female and 34 of them were male and thus, there were about twice the number of female responents compared to the male ones.
Figure : Distribution of the respondents by religion
As expected, the number of muslin respondents were highest, numbering up to 76. Other tan them, there were 16 hindu respondents and 4 respondents who followed buddhism and christinity, together totalling to 8
Figure : Distribution of the respondents by marital status
There were 86 married respondents and 14 unmarried ones.
Figure : Distribution of the respondents by education
The majority of the respondents had studied up to completing their HSCs (22) or up to their SSCs (18). There were also 14 respondents who studied up to class V (or below) and also 14 who had left their studies between the classes of VI to X. A small number (12) of them had completed their Masters courses and only 2 of them had completed higher education courses and degrees above Masters (PhD etc.).
Figure : Distribution of the respondents by occupation
The service sector was the employer of the largest number of respondents (44). There were other positions which the rest of the respondents were employed in (in small numbers) such as being a maid (6), garments worker (6), tailor (4), say labor (4) and also others (2). 4 of the respondents were self employed, owning small businesses (4), 6 were students and 30 of the female ones were housewives.
Table : Distribution of the respondents by the number of family member
| Frequency | Percent | |
| 2 | 6 | 6.0 |
| 3 | 20 | 20.0 |
| 4 | 40 | 40.0 |
| 5+ | 34 | 34.0 |
| Total | 100 | 100.0 |
Most of the respondents lived in families of average sizes of 4 (40) and 3 (20) although 34 of them have families with 5 or more members. A minor number of the respondents had family sizes of two.
Figure : Distribution of the respondents by ever heard about HIV/AID
About all the respondents had heard of AIDS (98) but two of them hadn’t.
Figure : Distribution of the respondents by knowledge about the protection becoming infected with HIV
Multiple responses
Based on multiple responses, the majority of the respondents (64) thought limiting sex only within marriage would prevent themselves from being infected with HIV/AIDS. Moderate amounts of them thought abstaining from having sex (30) and wearing a condom (34) would prevent the spread of HIV. A few respondents thought of ideas such as avoiding unscreened blood transfusion (4) and preventing the use of non-sterile syringes (4) would prevent them from being subject to HIV/AIDS
Table : Distribution of the respondents by attitude towards HIV through following statements
Yes | No | Don’t know | ||||
n | % | n | % | n | % | |
| It is possible for a healthy looking person to have HIV infection | 80 | 80.0 | 20 | 20.0 | ||
| People can reduce their chance of getting the AIDS virus by having just one uninfected sex partner who has no other sex partner | 78 | 78.0 | 4 | 4.0 | 18 | 18.0 |
| People can get the AIDS virus from mosquito bites | 10 | 10.0 | 68 | 68.0 | 22 | 22.0 |
| People can reduce their chance getting the AIDS virus by using a condom every time they have sex | 64 | 64.0 | 18 | 18.0 | 18 | 18.0 |
| People can get the AIDS virus by sharing food with a person who has AIDS | 6 | 6.0 | 80 | 80.0 | 14 | 14.0 |
| People can get the AIDS virus by using unsterilized needle of syringe | 14 | 14.0 | 78 | 78.0 | 8 | 8.0 |
| Can people get the AIDS virus through unsafe blood transfusion | 90 | 90.0 | 10 | 10.0 | ||
| People can reduce their chance of getting the AIDS virus by not having sexual intercourse at all | 84 | 84.0 | 10 | 10.0 | 6 | 6.0 |
| Suppose or your close relative or friend has AIDS. Do you agree to look after him/ her | 84 | 84.0 | 2 | 2.0 | 14 | 14.0 |
Upon being asked questions to check the respondents’ knowledge of HIV/AIDS, most of the people’s answers were correct and showed that most of them were properly aware of the situation. Some of them were aware, but needed to know more to info on the subject. Some of them though, literally knew nothing about HIV/AIDS at all.
Table : Distribution of the respondents by ever heard about STI other than HIV/AIDS
| Frequency | Percent | |
| Yes | 94 | 94.0 |
| Don’t know | 6 | 6.0 |
| Total | 100 | 100.0 |
The max number of respondents had about STIs other than HIV/AIDS (94) but 6 of them were still to learn of any.
Table : Distribution of the respondents by knowledge about the name of STD
Frequency | Percent | |
| Syphilis | 82 | 82.0 |
| Gonorrhea | 38 | 38.0 |
| Chlamydia | 2 | 2.0 |
| Genital herpes | 4 | 4.0 |
| Don’t know | 4 | 4.0 |
Multiple responses
A large number of respondents knew about sexually transmitted diseases such as syphilis (82) and Gonorrhea (38). Only a few of them knew about chlamydia (2) and genital herpes (4). 4 of the respondents were completely unaware of any STDs.
Table : Distribution of the respondents by knowledge about the Sign and symptoms to indicate a man is suffering from STD
Frequency | Percent | |
| Pus discharge from urethra | 50 | 50.0 |
| Ganital ulcer | 34 | 34.0 |
| Itching in genitalia | 66 | 66.0 |
| Warts on genitalia | 18 | 18.0 |
| Burning sensation during micturition | 50 | 50.0 |
| Swelling on groin area | 34 | 34.0 |
| Pain/ swelling of scrotum/ testis | 58 | 58.0 |
| Others | 2 | 2.0 |
| Don’t know | 12 | 12.0 |
Multiple responses
Based on multiple responses, average numbers (30-66) of respondents were aware of most symptoms of men’s STDs, some of them being common e.g., itching on the genitalia (66) and burning sensation during micturition. Only 2 of the respondents knew about other rarer symptoms while 12 knew none.
Table : Distribution of the respondents by knowledge about the Sign and symptoms to indicate a woman is suffering from STD
Frequency | Percent | |
| Lower abdominal pain | 76 | 76.0 |
| Vaginal discharge | 58 | 58.0 |
| Foul smelling discharge | 64 | 64.0 |
| Burning/ pain on urination | 32 | 32.0 |
| Genital ulcer/ sores | 2 | 2.0 |
| Swelling on groin area | 26 | 26.0 |
| Pain during intercourse | 56 | 56.0 |
| Genital warts | 4 | 4.0 |
| Bleeding during intercourse | 40 | 40.0 |
| Don’t know | 10 | 10.0 |
Multiple responses
Based on multiple responses, average to high numbers of respondents were aware of most of the symptoms of women’s STDs. 10 of them did not know of any symptoms and only some knew of symptoms such as genital warts (4), genital ulcers/sores (2).
Figure : Distribution of the respondents by knowledge about person should be treated when s/he is infected with STI
Half of the total respondents said they would treat only the person suffering from the STD but 44 of them said they would treat the couple altogether. 6 people were unsure.
Table : Distribution of the respondents by knowledge about the Outcomes of untreated STI
Frequency | Percent | |
| Infertility | 58 | 58.0 |
| Prone to HIV/AIDS infection | 46 | 46.0 |
| Still birth | 16 | 16.0 |
| Abortion or miscarriage | 26 | 26.0 |
| Spontaneous abortion | 36 | 36.0 |
| Ectopic pregnancy/ conception other than uterus | 14 | 14.0 |
| New born can be blind | 10 | 10.0 |
| Partner can be infected | 52 | 52.0 |
| Death | 6 | 6.0 |
| Don’t know | 16 | 16.0 |
Multiple responses
Highest numbers of respondents knew that an untreated STI can eventually lead to cases such as infertility (58), partner also receiving the infection (52), spontaneous abortion (36), being prone to infection of HIV/AIDS (46) and abortion/miscarriage (26). Relatively few of the respondents knew of hazards such as ectopic pregnancy/conception other than uterus (14), newborn being blind (10) and still birth (16). 16 people had no information about the final circumstances of an untreated STI.
Table : Distribution of the respondents by knowledge about the Prevention of STI
Frequency | Percent | |
| Abstain from sex | 52 | 52.0 |
| Have only one sexual partner | 40 | 40.0 |
| Limit sex only within marriage | 72 | 72.0 |
| Use condom during sex | 82 | 82.0 |
| Avoid unscreened blood transfusion | 48 | 48.0 |
| Avoid using non-sterile syringes | 54 | 54.0 |
| Don’t know | 2 | 2.0 |
Multiple responses
Based on multiple responses, the majority of the respondents thought limiting sex only within marriage (72), using condoms during sex (82), preventing the use of non-sterile syringes (54) and abstaining from having sex (52) would prevent themselves from being infected with HIV/AIDS. Moderate amounts of them thought avoiding unscreened blood transfusion (48) and having only one sexual partner (40) would prevent the spread of HIV. In this case, only 2 respondents had no concept upon the subject.
Table : Distribution of the respondents by knowledge about what a person should do if s/he suffers from STI
Frequency | Percent | |
| Seek treatment from a qualified doctor | 90 | 90.0 |
| Instructions of doctor should be strictly followed | 74 | 74.0 |
| One should complete the full course of medicine even if symptoms disappeared | 40 | 40.0 |
| Both partners should receive the treatment | 66 | 66.0 |
| Receive treatment from traditional healers | 6 | 6.0 |
| Don’t know | 2 | 2.0 |
Multiple responses
Based on multiple responses, the peak quantity of respondents (obviously) thought a qualified doctor should be consulted (90) and his instructions should be strictly followed (74) if one was infected by an STI. A number of respondents expressed that they would complete the full course of medicine to cure the STI even if symptoms disappear (40) and some thought it would be best if both partners received treatment (66). A few of the respondents think that receiving treatment from traditional doctors/healers would solve their problems (6) and 2 were unaware of what to do.
Table : Distribution of the respondents by knowledge about Sources of information
Frequency | Percent | |
| UHC | 34 | 34.0 |
| HFWC | 16 | 16.0 |
| Sattelite clinics/ EPI outreach | 2 | 2.0 |
| Doctors/ service providers | 20 | 20.0 |
| NGO clinic | 4 | 4.0 |
| Field workers | 14 | 14.0 |
| Community leaders | 6 | 6.0 |
| Counselors | 2 | 2.0 |
| Adolescent facilitators | 2 | 2.0 |
| Friends/ peer educators | 28 | 28.0 |
| Poster/ leaflet/ brochure | 42 | 42.0 |
| Book/ newspaper/ magazine | 12 | 12.0 |
| Bill board/ sign board | 2 | 2.0 |
| Radio | 48 | 48.0 |
| TV | 94 | 94.0 |
Multiple responses
As for sources of information, most respondents relied upon for knowledge/heard about HIV/AIDS from the TV (94), radio (48) and posters/leaflets/brochures (42). There were also many other sources which provided information about HIV/AIDS to small numbers of respondents.
Table : Distribution of the respondents by Recommendation to improve knowledge
Frequency | Percent | |
| Training on HIV/ AIDS | 80 | 80.0 |
| Include it in the nursing curriculum | 34 | 34.0 |
| Regular refresher for updating knowledge | 28 | 28.0 |
| Others | 12 | 12.0 |
Multiple responses
Based on multiple responses, the majority of the respondents suggested training on HIV/AIDS (80) could improve knowledge on the subject. Groups of respondents also suggested including it in the nursing curriculum (34) and regular refreshers for updating knowledge (28).
Discussion
In the study, out of the 100 repondents, 66 of them were female and 34 of them were male and thus, there were about twice the number of female responents compared to the male ones. As expected, the number of Muslim respondents were highest, numbering up to 76. Other tan them, there were 16 Hindu respondents and 4 respondents who followed Buddhism and Christinity, together totalling to 8. There were 86 married respondents and 14 unmarried ones. The majority of the respondents had studied up to completing their HSCs (22) or up to their SSCs (18). There were also 14 respondents who studied up to class V (or below) and also 14 who had left their studies between the classes of VI to X. A small number (12) of them had completed their Masters courses and only 2 of them had completed higher education courses and degrees above Masters (PhD etc.).
The service sector was the employer of the largest number of respondents (44). There were other positions which the rest of the respondents were employed in (in small numbers) such as being a maid (6), garments worker (6), tailor (4), say labor (4) and also others (2). 4 of the respondents were self employed, owning small businesses (4), 6 were students and 30 of the female ones were housewives. Most of the respondents lived in families of average sizes of 4 (40) and 3 (20) although 34 of them ha families with 5 or more members. A minor number of the respondents had family sizes of two. About all the respondents had heard of AIDS (98) but two of them hadn’t.
Based on multiple responses, the majority of the respondents thought limiting sex only within marriage would prevent themselves from being infected with HIV/AIDS. Moderate amounts of them thought abstaining from having sex (30) and wearing a condom (34) would prevent the spread of HIV. A few respondents thought of ideas such as avoiding unscreened blood transfusion (4) and preventing the use of non-sterile syringes (4) would prevent them from being subject to HIV/AIDS. “The awareness of HIV/AIDS in the Bangladeshi population remains quite low. One recent survey found that “Only 19 percent of ever-married women and 33 percent of currently married men had heard of AIDS.”
Upon being asked questions to check the respondents’ knowledge of HIV/AIDS, most of the people’s answers were correct and showed that most of them were properly aware of the situation. Some of them were aware, but needed to know more to info on the subject. Some of them though, literally knew nothing about HIV/AIDS at all. The max number of respondents had about STIs other than HIV/AIDS (94) but 6 of them were still to learn of any. “The proportion having knowledge on the prevention of HIV/AIDS was almost equal between the male and the female, except the use of condom during sex”.
A large number of respondents knew about sexually transmitted diseases such as syphilis (82) and Gonorrhea (38). Only a few of them knew about chlamydia (2) and genital herpes (4). 4 of the respondents were completely unaware of any STDs. Based on multiple responses, average numbers (30-66) of respondents were aware of most symptoms of men’s STDs, some of them being common e.g., itching on the genitalia (66) and burning sensation during micturition. Only 2 of the respondents knew about other rarer symptoms while 12 knew none. “With regard to basic knowledge of HIV/AIDS, 79% could tell the commonest mode of HIV transmission and 146 (53%) could describe window period correctly. 74% knew the full form of HIV. Less than half, 115 (42%) were able to identify the best method of prevention (maybe the question was poorly framed). Less than half, 134, (48%) could tell the common major signs that help in provisional diagnosis of AIDS.”
Based on multiple responses, average to high numbers of respondents were aware of most of the symptoms of women’s STDs. 10 of them did not know of any symptoms and only some knew of symptoms such as genital warts (4), genital ulcers/sores (2). Half of the total respondents said they would treat only the person suffering from the STD but 44 of them said they would treat the couple altogether. 6 people were unsure. Highest numbers of respondents knew that an untreated STI can eventually lead to cases such as infertility (58), partner also receiving the infection (52), spontaneous abortion (36), being prone to infection of HIV/AIDS (46) and abortion/miscarriage (26). Relatively few of the respondents knew of hazards such as ectopic pregnancy/conception other than uterus (14), newborn being blind (10) and still birth (16). 16 people had no information about the final circumstances of an untreated STI.
Based on multiple responses, the majority of the respondents thought limiting sex only within marriage (72), using condoms during sex (82), preventing the use of non-sterile syringes (54) and abstaining from having sex (52) would prevent themselves from being infected with HIV/AIDS. Moderate amounts of them thought avoiding unscreened blood transfusion (48) and having only one sexual partner (40) would prevent the spread of HIV. In this case, only 2 respondents had no concept upon the subject. Based on multiple responses, the peak quantity of respondents (obviously) thought a qualified doctor should be consulted (90) and his instructions should be strictly followed (74) if one was infected by an STI. A number of respondents expressed that they would complete the full course of medicine to cure the STI even if symptoms disappear (40) and some thought it would be best if both partners received treatment (66). A few of the respondents think that receiving treatment from traditional doctors/healers would solve their problems (6) and 2 were unaware of what to do.
As for sources of information, most respondents relied upon for knowledge/heard about HIV/AIDS from the TV (94), radio (48) and posters/leaflets/brochures (42). There were also many other sources which provided information about HIV/AIDS to small numbers of respondents. Based on multiple responses, the majority of the respondents suggested training on HIV/AIDS (80) could improve knowledge on the subject. Groups of respondents also suggested including it in the nursing curriculum (34) and regular refreshers for updating knowledge (28).
Conclusion
HIV/AIDS has created a major global health crisis. The UNAIDS and the World Health Organization (WHO) Epidemic update (December 2002) reflected a grim reality-the estimated number of people living with HIV/AIDS by the end of 2002 was 42 million. Nearly two-thirds of them live in Sub-Saharan Africa, where in the two hardest hit countries HIV prevalence is almost 40%. The global HIV/AIDS epidemic killed more than 3 million people in 2003 and there are emerging and growing epidemics in China, Indonesia, Papua New Guinea, Vietnam, several Central Asian Republics, the Baltic States, and North Africa. In Bangladesh, the disease is not yet epidemic but due to unaware status and less protective sexual behavior it could be outburst if the people are not aware about it.
There is lack of knowledge among the people about STIs in Bangladesh. Study findings also show that only 25 percent of the male and five percent of the female adolescents were aware of STIs, except HIV. Half of the male and a little over one-fourth of the female adolescents mentioned avoiding sex with an STI-infected person as a way of preventing STIs. About a similar proportion of the male and female mentioned use of condom during sex as a preventive measure. The rural male adolescents were more likely to have knowledge about the ways of preventing STIs than their urban counterparts. The Bangladesh Demographic and Health Survey (BDHS), 2004 showed that about a four-fifth of currently married men did not have any knowledge of STIs and only one-tenth knew about two or more symptoms of STIs. So, it is necessary to raise the knowledge of the people about HIV/AIDS.
Recommendations
After analyzing the study findings, the study recommends the following.
- By analyzing the findings it could be recommended that awareness raising program on HIV/AIDS and STDs for the people need to be strengthening effectively to make the people more aware about detail about HIV/AIDS and STDs.
- The findings stated that most of the respondents get HIV/AIDS and STDs information from the Upazila Health Complex and from the field level government health staff. So, the staff working in these levels could be trained to provide more knowledge to the people. Intervention to train the health service providers could be effective in this regard. So, mechanism can be developed to train the health service providers and dissemination of that message among the people.
- Partial knowledge is sometime harmful for the people especially if it is about disease. The people found partial knowledgeable with some wrong perception about HIV/AIDS and STDs. Before designing any program in this regard this findings could be considered.