Because of how swiftly COVID-19 spread over the globe, it became clear that we require more effective ways to quickly and accurately diagnose infectious diseases.
Polymerase chain reaction (PCR) testing were one of the most frequently utilized methods to identify COVID-19 in the early months of the pandemic. These viral RNA-based methods are less than ideal for point-of-care testing since they call for pricey apparatus and have lengthy reaction times (more than an hour).
The limitations of PCR stimulated the development of many immunoassay techniques, which employ specifically tailored antibodies to quickly and sensitively identify SARS-CoV-2 antigens. Immunoassay technology is continually being improved by scientists today to make accessible techniques more practical, sensitive, and economical.
In light of this, a group of scientists at Tokyo Institute of Method (Tokyo Tech), Japan, under the direction of Professor Hiroshi Ueda, have been developing a potential new technology for detecting COVID-19 and perhaps other infectious disorders. In addition to describing a new Quenchbody fluorescent immunosensor that can detect SARS-CoV-2 with exceptional speed and sensitivity, their most recent paper, which was published in Analyst, also outlines a straightforward method to significantly improve the immunosensor’s performance by using a crowding agent.
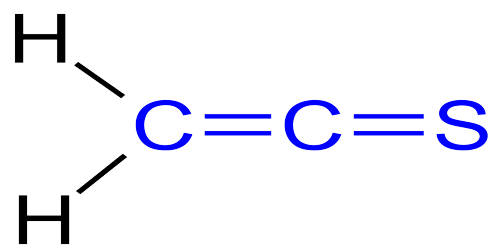
But what are Quenchbodies exactly? Using fluorescent tags and antibody fragments, Professor Ueda and colleagues created the first Quenchbody, a molecular sensor. A particular viral molecule (antigen) is targeted by the antibody fragment, which can be an antigen-binding region (or “Fab”).
Our work shows the feasibility of using Quenchbody immunosensors as rapid and cost-efficient tools for the diagnosis and high-throughput analysis of swab samples in large-scale monitoring and epidemiological studies of COVID-19, as well as other emerging infectious diseases.
Professor Hiroshi Ueda
The fluorescent tags, meanwhile, are tiny fluorescent dye molecules joined to the Quenchbody close to the antigen-binding site by a peptide linker. The fluorescent tags are drawn to the Fab in the absence of the antigen, and intrinsic amino acids, primarily tryptophan, interact with the dyes to squelch the fluorescence.
The fluorescent tag at the Fab is, however, replaced when the antigen shows up, prompting it to migrate away and regain its fluorescence. Thus, a rise in fluorescence during a Quenchbody test shows the presence of the target antigen.
The research team created a double-tagged Quenchbody in this work that specifically targets the SARS-CoV-2 nucleocapsid protein (N protein). They also investigated whether several commercially available chemicals may increase the sensitivity and response time of the immunosensor.
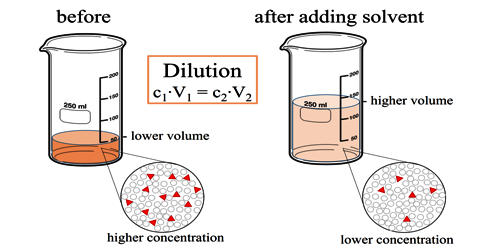
In particular, adding polyethylene glycol 6000 (PEG6000) at the right concentration as a crowding agent increased performance quite significantly.
“The enhanced limit of detection against the N protein was lower than 0.3 nM within 5 minutes of incubation, which is an order of magnitude more sensitive than without adding a crowding agent,” remarks Professor Ueda.
The team tested their immunosensor using unused clinical samples from COVID-19 positive patients to further confirm their strategy. After carefully examining the data, they came to the conclusion that their recently created Quenchbody could quantify and easily assess N protein in comparison to a commercial lateral flow antigen test.
Excited about these findings, Professor Ueda concludes: “Our work shows the feasibility of using Quenchbody immunosensors as rapid and cost-efficient tools for the diagnosis and high-throughput analysis of swab samples in large-scale monitoring and epidemiological studies of COVID-19, as well as other emerging infectious diseases.”
The back cover of Issue 22 of the magazine as well as the Analyst HOT Articles 2022 collection both highlight this study. We can only hope that this will assist Quenchbody technology gain more attention so that we are better equipped to handle pandemics in the future.