Alzheimer’s disease is the most common type of dementia, which is characterized by progressively deteriorating memory and other cognitive abilities. It has risen to the top of the list of main causes of death in recent decades. It can also shorten the length of a working career, cause uncertainty in retirement planning, and deprive patients of fun and satisfaction in their final years. An effective treatment for this disease could restore the patient’s ability to choose when to retire and improve the quality of life in old age.
Scientists at Temple University’s Alzheimer’s Center at the Lewis Katz School of Medicine are now on the hunt for a promising new therapeutic target: ABCA7, a protein known to defend against Alzheimer’s disease. The research, which was published online in the journal Cells, sheds fresh light on the link between ABCA7, cholesterol, and inflammation in human brain cells.
ABCA7’s role in the development of Alzheimer’s disease was first discovered in genome-wide association studies, which are huge studies of the human genome including thousands of people. “However, genome studies only point to a protein and do not tell us anything about how it functions or how it affects a disease,” said Joel Wiener, an investigator with Temple University’s Alzheimer’s Center and the study’s first author. “Our goal is to reveal ABCA7’s functions and to use what we learn about its role in pathology to turn it into an effective therapy against Alzheimer’s disease.”
Our findings suggest that cholesterol deficiency downregulates ABCA7 in many human brain cells. Previous research in mice demonstrated that cholesterol loss upregulates ABCA7. Other researchers discovered that inflammation suppresses ABCA7 in astrocytes, and we now show that this can also happen in microglia.
Mr. Wiener
Previous research performed by Nicholas Lyssenko, Ph.D., an investigator at Temple’s Alzheimer’s Center and corresponding author on the new paper, revealed that people between the ages of 63 and 78 who had low ABCA7 protein levels in the brain are more likely to acquire Alzheimer’s disease. This discovery supported previous genome research findings and suggested that the protein protects the human brain.
In the new study, Dr. Lyssenko’s team addressed how cholesterol metabolism and inflammation may manipulate ABCA7 levels in human brain cells and thus affect Alzheimer’s disease pathogenesis. In one set of experiments, the researchers depleted cholesterol in different neural cell lines, such as microglia, astrocytes, and neurons, and then treated the cells with rosuvastatin, a medication that suppresses cholesterol synthesis. To determine the effect of inflammation on ABCA7, the team carried out another set of experiments in which the same cell lines were treated with one of three major proinflammatory cytokines: IL-1β, IL-6, or TNFα. Cytokines are small molecules that can trigger inflammation following their secretion from certain types of immune cells.
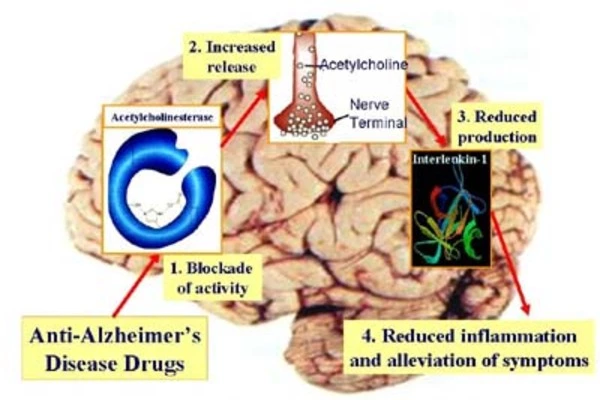
The researchers found that ABCA7 levels dropped by about 40 percent in microglia cell lines and about 20 percent in an astrocyte cell line after the cells were depleted of more than half their usual amount of cholesterol. Meanwhile, no changes were observed in ABCA7 levels in a neuronal cell line following cholesterol loss. In addition, IL-1β and TNFα suppressed ABCA7 expression only in microglial cells. The third cytokine, IL-6, had no impact on ABCA7 in microglia, and none of the three cytokines induced changes in ABCA7 levels in either astrocytes or neurons.
These findings contribute to a better understanding of how ABCA7 is regulated in the brain. “Our findings suggest that cholesterol deficiency downregulates ABCA7 in many human brain cells. Previous research in mice demonstrated that cholesterol loss upregulates ABCA7,” Mr. Wiener explained. “Other researchers discovered that inflammation suppresses ABCA7 in astrocytes, and we now show that this can also happen in microglia. Overall, cholesterol depletion and inflammation may lower ABCA7 levels in the brain, causing Alzheimer’s disease to develop.”
The Temple team is examining ABCA7 in a variety of ways, including employing not only human cells but also animal models and postmortem human brain tissue. “The greatest challenge now is to figure out how to measure ABCA7 levels in the brain of living humans,” he said. “If we succeed, we will be able to test whether inflammation suppresses ABCA7 in the human body.” Effective testing for ABCA7 levels in the brain will help identify those who are more likely to acquire Alzheimer’s disease and encourage the development of new ABCA7-based therapeutics.”