A research team set out to investigate the variety and biological processes of human Th2 cells. They identified a subpopulation of Th2 cells known as Th2-MPP cells after analyzing gene expression in inflamed regions. Their findings suggested that these cells could act as progenitors to numerous critical Th2 cell populations responsible for illness symptoms. These findings pave the way for therapeutic therapies targeting these cells, which could provide relief to people suffering from allergies.
Currently, the majority of allergic illness treatments are lifelong. Allergic reactions, which are characterized by persistent (type 2) inflammation in response to prolonged antigen exposure, are at the root of many chronic diseases in humans, including asthma, atopic dermatitis, and ulcerative colitis. T helper 2 (Th2) cells are vital in the body’s immunological response, especially in allergic reactions. Despite their critical significance, Th2 cells’ persistent activity during allergic reactions, especially in the face of continual antigen exposure, has long perplexed researchers.
Our work suggests that Th2-MPP cells have the potential to sustain type 2 inflammation in the face of chronic antigen exposure and lays the foundation for further investigation to better understand their contribution to disease.
Radomir Kratchmarov
A research team that included authors from Mass General Brigham, including members Brigham and Women’s Hospital, Massachusetts General Hospital, and Mass Eye and Ear, embarked on a quest to understand the diversity and cellular mechanisms of human Th2 cells. By conducting gene expression analyses of inflamed tissues, they pinpointed a subset of Th2 cells called Th2-MPP cells.
Their findings suggested that these cells might serve as precursors to several crucial Th2 cell populations responsible for disease symptoms. These discoveries lay the groundwork for therapeutic interventions targeting these cells, potentially offering relief to patients living with allergic diseases. Results are published in Nature Immunology.
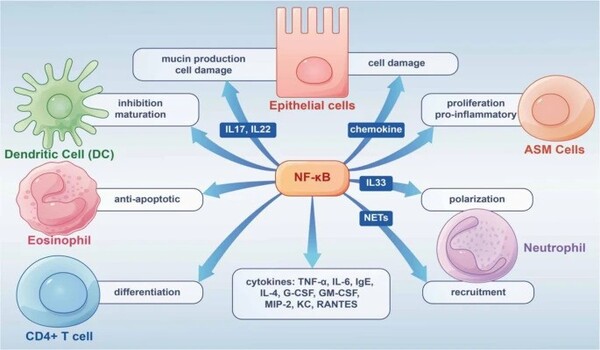
The researchers constructed a single-cell transcriptomic atlas, a comprehensive database of genes that are turned “on” and “off” in individual cells in the body, using inflamed tissues from patients with nine different chronic allergic illnesses. This atlas was utilized to identify Th2-multipotent progenitor (Th2-MPP) cells that consistently expressed two transcription factors, TCF7 and LEF1.
These transcription factors enabled Th2-MPP cells to behave similarly to stem cells in cancer and chronic infection, serving as progenitor cells capable of giving rise to different types of cells. The researchers also investigated Th2 cells from nasal tissue in patients with chronic rhinosinusitis. They discovered that Th2-MPP cells could be the precursors to many types of Th2 cells that generate illness symptoms.
“We still have much to learn about the contribution of progenitor cells to chronic human inflammation, but we are hopeful that the study of this area of immunity could provide opportunities for future disease-modifying therapeutic approaches,” said senior author Patrick Brennan, MD, PhD, a physician-researcher in the Brigham Division of Allergy and Clinical Immunology.
“Our work suggests that Th2-MPP cells have the potential to sustain type 2 inflammation in the face of chronic antigen exposure and lays the foundation for further investigation to better understand their contribution to disease,” said lead author Radomir Kratchmarov, MD, a research fellow in the Brigham Division of Allergy and Clinical Immunology.