Periodontitis
Definition
Periodontitis is a serious gum infection that damages the soft tissue and bone that supports the tooth. The word “periodontitis” literally means “inflammation around the tooth.” Periodontitis involves progressive loss of the alveolar bone around the teeth, and if left untreated, can lead to the loosening and subsequent loss of teeth. All periodontal diseases, including periodontitis, are infections which affect the periodontium.
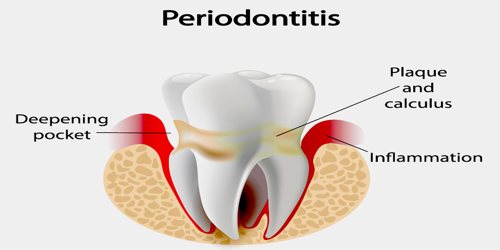
Periodontitis and all periodontal diseases are bacterial infections that destroy the attachment fibers and supporting bone that hold the teeth in the mouth. Left untreated, these diseases can lead to tooth loss. The main cause of periodontal disease is a bacterial plaque, a sticky, colorless film that constantly forms on teeth.
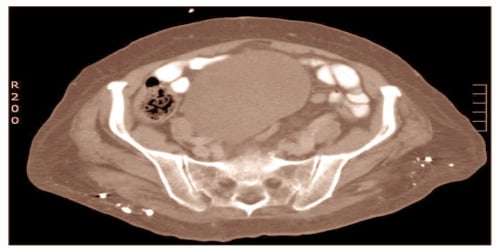
Untreated periodontitis will eventually result in tooth loss and may increase the risk of stroke, heart attack, and other health problems. Bacterial plaque, a sticky, colorless membrane that develops over the surface of teeth, is the most common cause of periodontal disease. A diagnosis of periodontitis is established by inspecting the soft gum tissues around the teeth with a probe and by evaluating the patient’s X-ray films, to determine the amount of bone loss around the teeth. Specialists in the treatment of periodontitis are periodontists; their field is known as “periodontology” or “periodontics”.
Causes, Sign, and Symptoms of Periodontitis
Periodontitis is caused by certain bacteria, which is also known as periodontal bacteria and by the local inflammation triggered by those bacteria. Although these periodontal bacteria are naturally present in the mouth, they are only harmful when the conditions are right for them to increase dramatically in numbers. This happens when a layer of bacteria and food debris, known as plaque, builds up and is left undisturbed on the teeth, commonly in hard-to-reach areas such as between the teeth.
A risk factor is something that increases the risk of developing a condition or disease. The following risk factors are linked to a higher risk of periodontitis:
- Smoking – regular smokers are much more likely to develop gum problems. Smoking also undermines the efficacy of treatments.
- Hormonal changes in females – puberty, pregnancy, and the menopause are moments in life when a female’s hormones undergo changes. Such changes raise the risk of developing gum diseases.
- Diabetes – patients who live with diabetes have a much higher incidence of gum disease than other individuals of the same age
- AIDS – people with AIDS have more gum diseases
- Cancer – Cancer and some cancer treatments can make gum diseases more of a problem
- Some drugs – some medications that reduce saliva are linked to gum disease risk.
- Genetics – some people are more genetically susceptible to gum diseases.
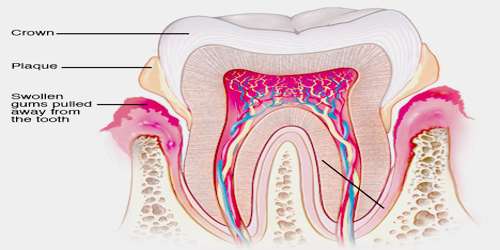
In the early stages, periodontitis has very few symptoms, and in many individuals, the disease has progressed significantly before they seek treatment.

Symptoms may include:
- Redness or bleeding of gums while brushing teeth, using dental floss or biting into hard food (e.g., apples)
- Gum swelling that recurs
- Spitting out blood after brushing teeth
- Halitosis, or bad breath, and a persistent metallic taste in the mouth
- Gingival recession, resulting in apparent lengthening of teeth. This may also be caused by heavy-handed brushing or with a stiff toothbrush.
- Deep pockets between the teeth and the gums
- Loose teeth, in the later stages
Periodontitis has been linked to increased inflammation in the body, such as indicated by raised levels of C-reactive protein and interleukin-6. It is linked through this to increased risk of stroke, myocardial infarction, and atherosclerosis.
Treatment and Prevention of Periodontitis
With careful assessment and treatment, it is usually possible to completely halt the progress of periodontitis. The key to success is to eliminate the bacterial plaque which is triggering the disease process and to establish excellent oral hygiene practices.
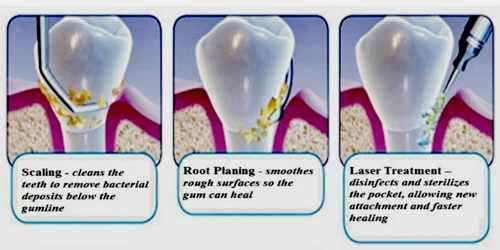
Initial treatment: It is important to remove plaque and calculus (tartar) to restore periodontal health.
Medications –
- Prescription antimicrobial mouthrinse – It controls bacteria when treating gum disease, as well as after surgery. Patients use it like they would a regular mouthwash.
- Antiseptic “chip” – this is a small piece of gelatin which is filled with chlorhexidine. It controls bacteria and reduces periodontal pocket size. This medication is placed in the pockets after root planing. The medication is slowly revealed over time.
- Antibiotic gel – a gel that contains doxycycline, an antibiotic. This medication controls bacteria and shrinks periodontal pockets. It is a slow-release medication.
- Antibiotic microspheres – miniscule particles containing minocycline, an antibiotic. It is also used to control bacteria and reduce periodontal pocket size. It is a slow-release medication.
- Enzyme suppressant – keeps destructive enzymes in check with a low-dose of doxycycline. Some enzymes can break down gum tissue; this medication holds back the body’s enzyme response. Taken orally as a pill, and is used with scaling and root planing.
- Oral antibiotics – either in capsule or tablet form and are taken orally. They are used short-term for the treatment of acute or locally persistent periodontal infection.
Periodontal inflammation is not inevitable. The development of gingivitis and periodontitis can be prevented by adopting thorough oral hygiene habits, alongside regular professional examinations and support.
The basic elements of a good oral hygiene regime are:
- Cleaning the chewing surfaces and sides of the teeth twice daily, with a toothbrush (of an appropriate size and in good condition) and toothpaste.
- Cleaning the spaces between the teeth where the toothbrush bristles cannot reach, using either dental floss or an interdental brush, depending on the size of the space. This should be done once daily.
The most common complication of periodontitis is the loss of teeth. However, patients with periodontitis are also at a higher risk of having respiratory problems, stroke, coronary artery disease, and low birth weight babies. Regular dental check-ups and professional teeth cleaning as required: Dental check-ups serve to monitor the person’s oral hygiene methods and levels of attachment around teeth, identify any early signs of periodontitis, and monitor response to treatment.
Reference: