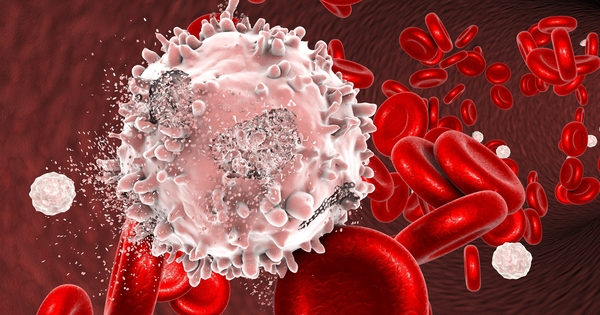
Blood cancer, also known as hematopoietic cancer, refers to several types of cancer that affect the blood, bone marrow, and lymphatic system. Leukemia, lymphoma, and multiple myeloma are examples. Advances in the detection and treatment of blood malignancies have been continuous, and new insights are emerging.
A groundbreaking study conducted by researchers from the Cancer Science Institute of Singapore (CSI Singapore) at the National University of Singapore (NUS) has revealed critical insights into the role of the histone methyltransferase NSD2 and its epigenetic target PKC in causing t(4;14) translocated multiple myeloma (MM), a high-risk subtype of blood cancer, to be more aggressive and resistant to treatment.
The study was led by Professor Wee Joo Chng, Senior Principal Investigator at CSI Singapore, and Dr Phyllis Chong Shu Yun, Senior Research Fellow at CSI Singapore. The research team discovered that NSD2 triggers elevated glycolysis through the activation of PKCα, leading to the production of excessive lactate that fuels malignancy and undermines response to immunomodulatory drugs. The findings present potential targets to improve the treatment of myeloma.
The goal of our research is to overcome the limitations of targeting the key deregulated gene in t(4;14) myeloma. It elucidates the metabolic reprogramming of MM in response to oxygen- and nutrient-depleted bone marrow microenvironment.
Prof Wee Joo Chng
Targets for therapeutic intervention
Myeloma is the second most common blood malignancy, with t(4;14) myeloma accounting for 15 to 20% of MM cases. Patients with t(4;14) myeloma have a poorer prognosis and a shorter overall survival when compared to other kinds of myeloma. Unfortunately, medicines cannot be used to target the primary unregulated gene in t(4;14) myeloma.
“The goal of our research is to overcome the limitations of targeting the key deregulated gene in t(4;14) myeloma. It elucidates the metabolic reprogramming of MM in response to oxygen- and nutrient-depleted bone marrow microenvironment. By investigating the epigenome and metabolome of NSD2, we sought alternative vulnerabilities that could revolutionize treatment strategies,” explained Prof Chng, the study’s principal author.
The novel link between NSD2 and cellular metabolism, mediated by histone methylation, opens up new possibilities in the fight against high-risk MM subtypes. The study has a wide-ranging impact, with the potential to influence the creation of new treatments and non-invasive diagnostic tools. Targeted metabolic therapies, whether through dietary changes or customized pharmaceutical approaches, could provide interesting therapeutic alternatives for patients with t(4;14) myeloma.
Furthermore, the fact that lactate levels can be used to predict treatment response underscores the transformational potential of metabolite signatures in personalized medicine.
Striving towards tailored interventions and personalized care
This work, which was published in Cancer Research, American Association for Cancer Research, represents a significant step forward in unraveling the complexity of MM and holds hope for improving treatment results for patients with high-risk subtypes.
In the future, Prof Chng and his colleagues intend to use the insights gathered from this work to develop therapeutic interventions for t(4;14) myeloma. The success of their metabolic characterization of t(4;14) myeloma also paves the way for the team to extend their metabolomic framework to profile other genetically high-risk MM subtypes such as t(14;16) or with 1q21 amplifications, paving the way for tailored interventions and personalized care.