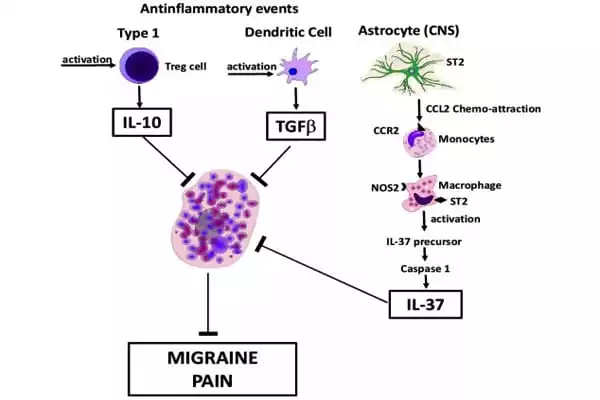
Older migraine theories indicated that symptoms were caused by variations in blood flow to the brain. Many headache researchers now believe that changes in blood flow and blood vessels do not cause pain, but may contribute to it. As enhanced technology and research have paved the path for a better understanding of migraine discomfort, current thought has shifted more toward the cause of the problem. Today, it is well accepted that chemical substances and hormones such as serotonin and estrogen frequently have a role in migraine pain sensitivity.
Migraines are a pain in the head and in the hip pocket, but newly discovered genetic causes by QUT researchers could lead the way to new preventative drugs and therapies.
Genetic analyses findings were published in The American Journal of Human Genetics by Professor Dale Nyholt and his PhD candidates Hamzeh Tanha and Anita Sathyanarayanan, all from the QUT Centre for Genomics and Personalised Health.
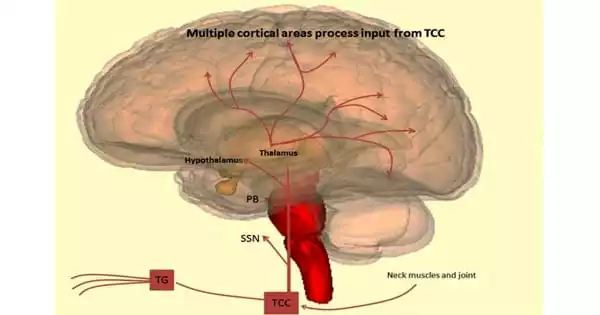
According to one component of migraine pain hypothesis, migraine pain is caused by waves of activity by groupings of excitable brain cells. These cause neurotransmitters like serotonin to constrict blood arteries. Serotonin is a neurotransmitter that is required for nerve cell transmission. It can cause blood vessel constriction throughout the body. Some people experience migraines when their serotonin or estrogen levels shift. Serotonin levels can impact both sexes, whereas estrogen levels only effect women.
Lower DHA levels are linked to inflammation, cardiovascular and brain problems such as depression, all of which are linked to migraine risk. Observed connections between genetic factors influencing blood metabolite levels and genetic risk for migraine suggest a modification of metabolites in migraine patients.
Professor Nyholt
Estrogen levels in women naturally fluctuate throughout their lives, increasing during reproductive years and decreasing afterwards. Monthly fluctuations in estrogen levels are also experienced by women of childbearing age. Migraines in women are frequently related with fluctuating hormone levels, which may explain why women are more likely than men to suffer from migraines.
Professor Nyholt said the team identified causal genetic links to three blood metabolite levels that increase migraine risk:
- lower levels of DHA, an omega-3 known to reduce inflammation
- higher levels of LPE(20:4), a chemical that blocks an anti-inflammatory molecule
- lower levels of a third, currently uncharacterised metabolite, named X-11315.
Professor Nyholt believes that future research and clinical trials could target these genetic linkages to design and test drugs that change metabolite levels and prevent migraine. He stated that migraine is predicted to cost the Australian economy $35.7 billion per year, and that current treatments fail up to 50% of migraine patients.
“Observed connections between genetic factors influencing blood metabolite levels and genetic risk for migraine suggest a modification of metabolites in migraine patients,” Professor Nyholt stated.
Metabolites are compounds produced or utilised by the body during the breakdown of food, medicines, or chemicals during metabolism. “Variations in blood levels of metabolites can be caused by diet, lifestyle, and heredity,” Professor Nyholt explained. “However, they are straightforward to assess and can be controlled by meal planning and supplementation.”
Except for docosahexaenoic acid (DHA), a very long-chain omega-3 that protects against migraine, patients with migraine had higher amounts of shorter length fatty acids, according to Professor Nyholt. “Fatty acids are composed of more complex lipids that aid in cell signaling, cell membrane composition, and gene expression, all of which influence disease risk,” he explained.
“Lower DHA levels are linked to inflammation, cardiovascular and brain problems such as depression, all of which are linked to migraine risk.” According to Professor Nyholt, LPE(20:4) is a chemical substance that inhibits the development of an anti-inflammatory molecule known as anandamide.
“If LPE(20:4) is managed to allow more anandamide to be produced to lower inflammation, this could potentially prevent migraine,” he explained. Lower blood levels of a third metabolite, X-11315, enhanced the risk of migraine, according to Professor Nyholt, and characterizing it is a subject of future research.