The fact that the most effective treatment cannot cross the blood-brain barrier to reach the aggressive brain tumor has been a significant hurdle to treating the lethal brain malignancy glioblastoma.
But now, researchers from Northwestern Medicine have released the findings of the first in-person clinical trial in which they broke down the blood-brain barrier and repeatedly penetrated important parts of the human brain to deliver chemotherapy that was injected intravenously using a novel, skull-implantable ultrasound device.
The patient is awake for the four-minute treatment to break down the blood-brain barrier, and after a few hours, they are sent home. The outcomes demonstrate that the therapy is secure and well tolerated, with some patients receiving up to six cycles.
The impact of blood-brain barrier opening caused by ultrasound on the levels of chemotherapy in the human brain has never been accurately measured before. The results demonstrated that opening the blood-brain barrier increased medication concentrations in the human brain by a factor of four to six.
With the help of the potent chemotherapy medicines paclitaxel and carboplatin, researchers were able to detect this rise. Because the medications do not normally cross the blood-brain barrier, they are not used to treat these patients.
Additionally, this is the first study to outline how soon sonication causes the blood-brain barrier to shut. The majority of blood-brain barrier restoration occurs within the first 30 to 60 minutes following sonication, the researchers found.
“The findings will allow optimization of the sequence of drug delivery and ultrasound activation to maximize the drug penetration into the human brain,” the authors said.
“This is potentially a huge advance for glioblastoma patients,” said lead investigator Dr. Adam Sonabend, an associate professor of neurological surgery at Northwestern University Feinberg School of Medicine and a Northwestern Medicine neurosurgeon.
In the past, studies that injected paclitaxel directly into the brain of patients with these tumors observed promising signs of efficacy, but the direct injection was associated with toxicity such as brain irritation and meningitis.
Dr. Adam Sonabend
“Temozolomide, the current chemotherapy used for glioblastoma, does cross the blood-brain barrier, but is a weak drug,” Sonabend said.
The paper will be published May 2, 2023, in The Lancet Oncology.
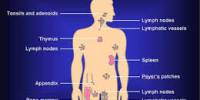
A tiny barrier known as the blood-brain barrier protects the brain from the vast majority of medications that are circulated. As a result, there is a relatively small selection of medications that can be utilized to treat brain disorders.
Most medications that are successful for cancer elsewhere in the body but do not penetrate the blood-brain barrier cannot be used to treat patients with brain cancer. Delivering medications to the brain is necessary for their effective repurposing to treat cancer and brain disorders.
“In the past, studies that injected paclitaxel directly into the brain of patients with these tumors observed promising signs of efficacy, but the direct injection was associated with toxicity such as brain irritation and meningitis,” Sonabend said.
Blood-brain barrier recloses after an hour
The researchers found that the blood-brain barrier may be temporarily opened in people using ultrasound and microbubble technology, and that most of its integrity returns an hour later.
“There is a critical time window after sonification when the brain is permeable to drugs circulating in the bloodstream,” Sonabend said.
The blood-brain barrier is fully restored 24 hours after brain sonication, according to prior human investigations. However, the field previously made the assumption that the blood-brain barrier is open during the first six to eight hours. The Northwestern study shows that this time window might be shorter.
In another first, the study reports that using a novel skull-implantable grid of nine ultrasound emitters designed by French biotech company Carthera opens the blood-brain barrier in a volume of brain that is nine times larger than the initial device (a small single-ultrasound emitter implant). This is crucial because for this method to be effective, a sizable area of the brain close to the cavity that remains after the excision of glioblastoma tumors must be covered.
Clinical trial for patients with recurrent glioblastoma
The study’s conclusions served as the foundation for a phase 2 clinical trial that researchers are currently running for patients with recurrent glioblastoma. The trial’s goal is to determine whether treating patients with paclitaxel and carboplatin at the same time and administering it to their brains using ultrasound technology lengthens their survival. A combination of these two drugs is used in other cancers, which is the basis for combining them in the phase 2 trial.
In the phase 1 clinical trial reported in this paper, patients underwent surgery for resection of their tumors and implantation of the ultrasound device. They started treatment within a few weeks after the implantation.
The blood-brain barrier opening associated with the three-weekly administration of paclitaxel was increased by researchers. Studies were carried out on specific patient populations during surgery to look at how this ultrasound equipment affected drug concentrations.
Fluorescein, a fluorescent dye, was used in the operating room to view and map the blood-brain barrier, and an MRI taken following ultrasonic therapy was also used.
“While we have focused on brain cancer (for which there are approximately 30,000 gliomas in the U.S.), this opens the door to investigate novel drug-based treatments for millions of patients who suffer from various brain diseases,” Sonabend said.
Other Northwestern authors include: A. Gould, C. Amidei, R. Ward, K. A. Schmidt, D.Y. Zhang, C. Gomez, J.F. Bebawy, B.P. Liu, I.B. Helenowski, R.V. Lukas, K. Dixit, P. Kumthekar, V. A. Arrieta. Lesniak, H. Zhang and R. Stupp.
The grants 1R01CA245969-01A1 and P50CA221747 from the National Cancer Institute of the National Institutes of Health and SPORE support from the Moceri Family Foundation and the Panattoni family fund this work.