Infectious diseases
At the beginning of the twentieth century, the major causes of death were infectious diseases caused by the infection of different bacteria, fungi or viruses. Still today infectious diseases are the second largest cause of mortality in the world accounting for more than 13 million deaths annually (C0hen, 2000). Control of infectious diseases has come as a result of comprehensive understanding of disease processes as well as improved sanitary practices and the discovery and use of antimicrobial agents. Bacteria belonging to the family Enterobacteriaceae are the most commonly encountered organisms isolated from clinical specimens (K. Islam). But pathogenic bacteria cause many of the diseases in human, animals and even in plants and insects. However, although we now live in a world where pathogenic microorganisms are under control, for the individuals dying slowly of acquired immune deficiency syndrome (AIDS), the cancer patient whose immune system has been devastated as a result if treatment with an anticancer drug, individuals infected with a multiply drug resistant pathogen, microorganism can still be the major threat to survival. Further, microbial diseases still constitute the major causes of death in many of the developing countries of the world (Cohen, 2000). Thus, microorganisms are still serious threats to human existence. But on the other hand we must emphasize that most microorganisms are not harmful to human. In fact, microorganisms do not cause harm to all and instead are actually beneficial, carrying out processes that are of immense value to human society. Even in the health care industry, microorganisms play beneficial roles. For instance, the pharmaceutical industry is a multibillion-dollar industry built in part on the large-scale production of antibiotics by microorganisms. A number of other major products are also derived, at least in part, from the activities of microorganisms (Kummerer, K. 2004).
Infectious diseases are the most common diseases of mankind and are a major source of morbidity and mortality in both developed and developing countries. Table-1.1 shows estimated morbidity and mortality figure for the common infectious diseases.
Table: – 1.1 Infectious diseases worldwide.
Disease | Estimated morbidity (No. Of cases in Thousands/year) | Estimated mortality (No. of deaths in thousands/year) |
Diarrhoeal disease | 2,000,000 – 5,000,000 | 10,000 |
Respiratory infection | – | 5,000 |
Malaria | 150,000 | 1,500 |
Schistosomiasis | 20,000 | 1,000 |
Whooping cough | 20,000 | 400 |
Neonatal tetanus | – | 150 |
(W. H. O. Report. 1998)
Mortality from infectious diseases
The World Health Organization (WHO) collects information on global deaths by International Classification of Disease (ICD) code categories. The following table-1.2 is the top infectious disease killers which caused more than 100,000 deaths in 2002 (estimated). Data obtained from the year 1993 is also included for comparison.
| 2002 | 1993 | ||||
| World population | 5.2 billion | 5.5 billion | 9.27% | ||
| Total deaths from all causes | 57 million | 8.51% | 51 million | ||
| Rank | Cause of death | Number | Percentage of total | Number | 1993 Rank |
| I. Communicable Diseases category | 14.9 million | 16.0% | |||
| 1 | Lower respiratory infections | 3.9 million | 6.8% | 4.1 million | 1 |
| 2 | HIV/AIDS | 2.8 million | 4.9% | 0.7 million | 7 |
| 3 | Diarrheal diseases | 1.8 million | 3.2% | 3.0 million | 2 |
| 4 | Tuberculosis (TB) | 1.6 million | 2.7% | 2.7 million | 3 |
| 5 | Malaria | 1.3 million | 2.2% | 2.0 million | 4 |
| 6 | Measles | 0.6 million | 1.1% | 1.1 million | 5 |
| 7 | Pertussis | 0.30 million | 0.5% | 0.36 million | 7 |
| 8 | Tetanus | 0.21 million | 0.4.% | 0.15 million | 12 |
| 9 | Meningitis | 0.17 million | 0.3% | 0.25 million | 8 |
| 10 | Syphilis | 0.16 million | 0.3% | 0.19 million | 11 |
| 11 | Hepatitis B | 0.10 million | 0.2% | 0.93 million | 6 |
| 12 | Tropical Diseases (6) | 0.13 million | 0.2% | 0.53 million | 9,10,16,17,18 |
(Note: The other categories of death are maternal and perinatal conditions (5.2%), nutritional deficiencies (0.9%), noncommunicable conditions (58.8%), and injuries (9.1%).)
Sources of infection
Source of infection mean normal growth habitats of microbes. Vehicles or reservoirs of infections are objects contaminated with live but non-growing microbes and are not source of infection. Following are the common source of infections:-
1. Patients:-Some infections are derived exclusively from human patients e.g. pulmonary tuberculosis, leprosy, syphilis, etc.
2. Carriers: – Carriers may spread disease like Diphtheria, typhoid fever and dysentery, etc.
3. Endogenous: – This occurs in carriers in potentially pathogenic bacteria when the invade sites other than normal habitats. A nasal carrier of pathogenic Staphylococci, for example, may become ill when these produce boils and wound infections at other sites.
4. Infected animals: – Infections from infected animals to man are called ‘zoonoses’. Examples are Bovine tuberculosis, anthrax, plague, etc.
5. Soil: – e.g. tetanus, gas-gangrene, maduromycosis and sporotrichosis etc.
Transmission of infectious diseases
Spread of infection usually takes place from one person to another person or animal that is either suffering from the disease or is a carrier. There are various modes by which infection may spread. The most important modes are states below:
(A) Physical contact
Direct contact
Physical contact can be direct contact without the intervention of intermediate objects. Diseases transmitted by this mode are generally termed as contagious diseases the most common examples of which are like gonorrhea, syphilis etc.
Indirect contact
In this mode, fomites like clothing’s, eating, utensils & other possessions are responsible for transmission. Spread of diphtheria may take place by this mode.
(B) Air-borne
Dust, droplets and droplet nuclei may carry viable infectious organisms and be responsible for spread of infections. Droplets of saliva, sputum and nasal secretions, during talking, coughing and sneezing are suspended in the air. It would be interesting to note that in one sneeze about 20,000 droplets suspended in air (M. R. Choudhury. 1986). Infection takes place when another person inhales droplets. Droplets spread whooping cough, tuberculosis, diphtheria, cerebrospinal meningitis, common cold and measles etc. Droplets falling on the ground or infected excreta in the dust may thus be responsible for spreading infection.
(C) Food-borne
Items of food or water may be contaminated with five infection transmitters which are faeces, flies, food, fluid, and finger.
(D) Insect-borne
Many infections are spread by insects. A number of viral diseases, rickettisial disease, bacterial diseases and protozoal diseases are transmitted through the agency of insects.
Routes of infection
In many diseases routes of infection are important because there are examples in which infection will not result unless the organisms are introduced by a particular route. Vibrio cholereae for example if inoculated subcutaneously will not cause diarrhoea (K. Islam. 2006).
Following are the routes through which microorganisms gain entrance to the body and cause specific disease.
A. Ingestion: – Contaminated food and drinks when ingested may cause infections. Examples are typhoid fever, food poisoning, dysenteries, cholera etc.
B. Inhalation: – Dusts, droplets etc. when inhaled may cause infection e.g. tuberculosis, cold, whooping cough etc.
C. Inoculation: – Intact skin offer resistance against bacterial infections. Microorganisms usually enter through some break in the continuity of skin e.g. minute abrasions, lacerations or puncture etc. However some organisms appear in penetrating intact skin e.g. Terponema pallidum. Insect victors are the common examples to introduce infections by their bites.
Microorganisms causing infectious diseases
Fungi
The fungi include the eukaryotic organisms commonly refer as to yeasts, which normally grow as single cells and molds, which grow in branching chains called hyphea. Fortunately, most fungi are harmless to humans, only about 50 species cause human disease, and the overall incidence of serious fungal infection if rather low, although certain superficial fungal infections are quite common (K. Islam. 2006).
Fungi cause disease through three major mechanisms. First, some fungi cause immune responses that can result in allergic, (hypersensitivity) reactions. For examples, Aspergillus spp. is a potent and common allergen often causing asthma and other hypersensitivity reactions.
A second fungal disease-producing mechanism involves the production and action of mycotoxins, a large, diverse group of fungal exotoxins. The best-known examples of mycotoxins, are produced by Aspergillus, an organism that commonly grows on improperly stores food such as grain. The toxins produced by such fungus are known as, which are highly toxic and induce tumors in some animals, especially in birds that feed on contaminated grain. Their direct role in human disease is not well defined (K. Islam. 2006).
A third fungal disease-producing mechanism is through infection. The growth of a fungus or on in the body is called a mycosis. Mycoses can range in severity from relatively innocuous, superficial diseases to serious, life-threatening diseases.
Virus
Viral diseases were however known even during the Pre-Christaintera. Many diseases whose origins were unknown have now been found to be due to viruses. At the moment there are about 200 obligate human viruses and about 50 known viral diseases that affect mankind (K. Islam. 2006).
Virus are unique group of living agent, extremely small in size, usually beyond the resolution of a light microscope, possess highest state of parasitism and may be responsible for a wide range of infection.
Viruses are infecting animals, plants and bacteria and accordingly they may be grouped under three main heads:
1. Animal viruses
2. Plant viruses
3. Bacterial viruses.
The last groups of viruses are known as bacteriophages or simply as phages.
Bacteria
The bacteria which are unicellular, prokaryotic, have important economical roles in the development of modern science and technology. Some bacteria are pathogenic and may cause many diseases for humans, animals, even plants and insects. Some are enteric and other is non-enteric. The Enterobacteriaceae are generally active fermenter of glucose an alcohol. All Enterobacteriaceae are found in the intestinal tract of human beings and other animals. In size Enterobacteriaceae commonly range from 0.5 to 2.0 mm in diameter and 1.0 to 10.0 mm in length (The organism of the family Enterobacteria may be divided into two major groups on the basis of fermentation end products of lactose, e.g. mixed acid, producers which include Escherichia coli, Shigella, Salmonella and Proteus, butylenes glycol-producers include three genera, Klebsiella, Enterobacter and Serratia).
Antibiotics
Antibiotics are substances which are produced by some microorganisms specially fungus and go against growth of other microorganisms. Many of them can be used as chemotherapeutic agents. Antibiotics also known as antimicrobial drugs are drugs that fight infections caused by bacteria. After their discovery in the 1940’s they transformed medical care and dramatically reduced illness and death from infectious diseases. However, over the decades the bacteria that antibiotics control have developed resistance to these drugs. Today, virtually all-important bacterial infections in the United States and throughout the world are becoming resistant. Antibiotic resistance can cause significant danger and suffering for children and adults who have common infections, once easily treatable with antibiotics. Antibiotic resistance has been called one of the world’s most pressing public health problems.
Mechanisms of action of antimicrobial drugs
In many instance the exact mechanism is not well understood. Indeed action of chemotherapeutic agent in vivo is very complex. Three main factors are to be taken into consideration. These are
A. Drug, B. Parasite and C. The host
In addition, with a particular drug more than one mechanism may involve for its antimicrobial activities. A brief outline of the probable mechanism of action of some of the important drug is given below:
- Inhibition of growth by competitive antagonism.
Many antibiotics such as sulpha group of drugs on act competitive antagonism. Synthesis of folic acid in bacteria is an important step in the ultimate synthesis of purines leading to DNA and RNA formation. Interference with folic acid metabolism will kill bacteria. For synthesis of folic acid PABA (para-aminobenzoic acid) is an essential metabolite (Azucena. 2006). Sulphonamides have structural similarity with PABA and therefore are called the analogues of PABA. Sulphonamide complex with PABA for the active center for enzyme and ultimately leads to the formation of nonfunctional folic acid analogues. Further growths of bacteria cell thus stops. Animal cells on the other hand do not synthesized folic acid. The compound has to come exogenous sources. Sulphonamide therefore cannot affect cellular growth in animals.
- Inhibition of cells wall synthesis
Almost all bacteria possess a cell wall, which is responsible for providing a corseting effect to the bacterial cell. If a bacterial cell without cell wall is not suspended in hypertonic environment it undergoes lysis. Penicillin is the antibiotic, which acts by inhibiting cell wall formation. In higher doses, complete inhibition of cell wall formation takes place whereas in low doses formation of dividing cross wall inhibited giving rise to bizarre large forms of bacteria. There are other antibiotics, which also inhibits bacterial cell wall formation. The examples are cephalosporines, bacitracin, vancomicin, novobiocin, cycloserine.
- Interference with cell membrane function
It performs vital functions particularly as a selective permeability barrier. Disruption of this delicate function will mean death to the cell. Antibiotics acting by disrupting the cell membrane functions are:
A. Polymyxin and B. Polyene antibiotics. Polymyxins acts on bacterial cell membrane particularly of the gram negative ones.
- Inhibition of protein synthesis
Mechanisms of protein synthesis in bacteria are not yet clearly defined and as such exact mode of action for any one antibiotic belonging to this group is not fully known. The examples of antibiotics, which act by inhibition of protein synthesis are chloramphenical, tetracyclin, streptomycin, rythromycin and lincomycin.
They interferes with
(a) the activity of 50S unit of bacterial ribosome,
(b) attachment of amino acids with nascent peptide chains and
(c) enzyme activity particularly that of peptidyl transferase.
(d) the binding of t-RNA to 30S unit of ribosome.
(e) amino acid by competing for binding sites in ribosome.
(f) the reading of mRNA message which leads to synthesis of non-functional proteins.
- Inhibition of nucleic acid synthesis
Actinomycin, mitomycin, 5-iodo-2’ deoxyuridine (5-IDU), quinolones are the drugs, which act by inhibition of DNA in the following way:-
Inhibition of DNA-Gyrase
↓
Inhibit uncoiling of super coil
↓
Inhibit DNA replication
Use of antibiotics in diseases
Almost all the infectious diseases are treated with antibiotics. A large variety of antibiotics have been produced and used to treat the infectious disease. The most common antibiotics that are used to combat the infection are as follows:-
Penicillins: – Bactericidal agents benzylpenicillin and penicillin V (oral) are used to treat infections caused by streptococci, pneumococci, clostridia and when sensitive, also staphylococcal infections, meningitis, gonorrhoea, syphilis and anthrax. Flucloxacillin and cloxacillin are used to treat beta-lactamase (Penicillinase) producing staphylococci, active against gram-positive bacteria (including enterococci) H. influenzae and many coliforms. Carbenicillin tocarcillin are useful in treating infections caused by P. aeruginosa. Azlocillin and penicillin are active against Klebsiellae and are also anti Pseudomonal (Jawetz. 1996).
Cephalosporins:- Like penicillin, cephalosporins are bactericidal and also have a beta-lactam ring. They are, however, stable to staphylococcal penicillinase and have broad-spectrum activity. They are less likely to cause hypersensitivity than penicillin. They are mainly used to treat severe systemic infections caused by aerobic Gram-negative organisms. They are expensive drugs. Some cephalosporins can damage the kidneys (Jawetz. 1996)
Glycopeptides:- Bactericidal I.V. administered expensive agents. Vancomycin is used to treat serious infection such as endocarditis and septicaemia caused by gram-positive bacteria, particularly multi-resistant strains (K. Islam. 2006).
Amino-glycosides: – Bactericidal, showing synergy with beta-lactam agents mainly reserved for the treatment of severe sepsis due to coliforms and other gram-negative aerobic bacilli. With beta-lactams, they are sometimes used to treat endocarditis caused by staphylococci and streptococci (Jawetz.1996).
Macrolides: – Useful bacteriostatic agents (may be bactericidal at high concentration), mainly used to treat staphylococcal infection, respiratory infections, non-specific urethritis and when indicated, Campylobacter enteritis. They are useful second-line drugs for treating patient with penicillin hypersensitivity. Resistance may occur with S. aureus, S. pyogens and S. pneumonia (K. Islam. 2006).
Lincosamide: – Useful in treating staphylococcal bone and joint infection and anaerobic infections, but lincosamide has been associated with Pseudomembranous colitis (K. Islam. 2006).
Chloramphenicol: – Bacteriostatic broad spectrum drug, used in treating typhoid fever, meningitis, rickettsial and chlamydial infection and also eye infection. It can cause aplastic anaemia and is toxic in neonates (Jawetz. 1996).
Tetracycline:- Bacteriostatic widely used broad-spectrum antibiotic with activity against gram-positive and some gram-negative bacteria and also borreliae, rickettsiae, chlamydiae, and mycoplasma. Resistance to tetracycline is common, e.g. with H.influenzae, S. pneumoniae and S. pyogenes. Proteus is always resistant (Jawetz. 1996).
Quinolones:- Bacteriostatic or bactericidal agents. Nalidixic acid is used to treat lower Gram-negative urinary infections. Ciprofloxacin (Fluroquinolone) is active against Pseudomonas and is also used to treat serious systemic infections (Jawetz. 1996).
Sulphonamides and trimethoprim:- Bacteriostatic agents (may be bactericidal in combination) with activity against gram positive and gram- negative organisms. Co-trimoxazole is used to treat urinary and respiratory tract infections, Pneumocystis pneumonia, and invasive salmonellosis. Many enterobacteria are resistant (Jawetz. 1996).
Metronidazole:- Bactericidal agent used to treat anaerobic infections, e.g. caused by bacteroides, anaerobic cocci and clostridia. Actinomyces are resistant. Also used to treat vincent’s angina and protozoal infection e.g. caused by T. vaginalis, E. histolytica, and G. lamblia (Jawtez. 1996).
Drug resistance
Since antibiotics and other antimicrobial drugs first became widely used in the World War II, they have saved countless lives and blunted serious complications of many feared diseases and infections. The success of antimicrobials against disease-causing microbes is among modern medicine’s great achievements. After more than 50 years of widespread use, however, many antimicrobials are not as effective as they used to be. Over time, some bacteria have developed ways to circumvent the effects of antibiotics. Widespread use of antibiotics is thought to have spurred evolutionarily adaptations that enable bacteria to survive these powerful drugs. Antimicrobial resistance provides a survival benefit to microbes and makes it harder to eliminate infections from the body. Ultimately, the increasing difficulty in fighting off microbes leads to an increased risk of acquiring infections in a hospital or other settings. Diseases such as tuberculosis, gonorrhea, malaria, and childhood ear infections are now more difficult to treat than they were just a few decades ago. Drug resistance is an especially difficult problem for hospitals harboring critically ill patients who are less able to fight off infections without the help of antibiotics. Heavy use of antibiotics in these patients selects for changes in bacteria that bring about drug-resistance. Unfortunately, this worsens the problem by producing bacteria with greater ability to survive even in the presence of our strongest antibiotics. These even stronger drug-resistant bacteria continue to prey on vulnerable hospital patients.
• Nearly 2 million patients in the United States get an infection in the hospital each year.
• About 90,000 of those patients die each year as a result of their infection, up from 13,300 patient deaths in 1992.
• More than 70 percent of the bacteria that cause hospital-acquired infections are resistant to at least one of the antibiotics most commonly used to treat them.
• People infected with antibiotic-resistant organisms are more likely to have longer hospital stays and require treatment with second- or third-choice medicines that may be less effective, more toxic, and more expensive.
In short, antimicrobial resistance is driving up heath care costs, increasing the severity of disease, and increasing the death rates from certain infections.
The fight between human and microbes continues. While Pharmaceutical scientists are discovering newer and more portent antimicrobial drugs, the pathogenic microbes, with their determination to survive are gaining resistance by various mechanisms. Indeed, microbial drug resistance is one of the most serious problems, which the human race is facing today. Drug resistance in bacterial population may be due to genetic or non-genetic mechanisms.
Mechanism of drug resistance
A. Genetic mechanisms
These may be of two types e.g. chromosomal and non-chromosomal.
- Chromosomal resistance
In a sensitive bacterial population, there may be a small number of drug resistance bacteria, which develops spontaneously as a result of mutation. Mutation is due to a change in a particular chromosomal locus.
- Extra chromosomal resistance
It will be realized that bacterial resistance just explain is due to change in the nature of a single bacterial gene in the chromosome. But now we know that this is not the state of affairs in all cases. More frequently resistance to particular drugs is due to the presence of additional genes in extra chromosomal DNA known as R-factors (Plasmid).
B. Non-Genetic Mechanisms
These may involve metabolic inactivity and loss target structures.
- Metabolic inactivity.
Organisms are more sensitive to a particular antimicrobial drug when they are actively multiplying and when their metabolic rate is high. They become relatively less sensitive or even insensitive to the same drug when they are metabolically inactive.
- Loss of target structures.
Resistance may be due to loss of target structures for drug actions. The best example of this type of resistance is that manifested by L-forms of bacteria to penicillin (Kotra. 2000).
A growing problem
For all these reasons, antibiotic resistance has been a problem for nearly as long as we’ve been using antibiotics. Natural selection of penicillin-resistant strains in a bacterium known as Staphylococcus aureus began soon after penicillin was introduced in the 1940s. Today, antibiotic-resistant strains of S. aureus bacteria as well as various enterococci are common and pose a global health problem in hospitals. More and more hospital-acquired infections are resistant to the most powerful antibiotics available, such as vancomycin. These drugs are reserved to treat only the most stubborn infections to slow development of resistance to them.
Sources of antibiotics and resistance in the environment
Hospital effluent
Antibiotics used in medicine for the treatment of infections and prophylactic are mainly released as non-metabolized into the aquatic environment via waste water. Unused therapeutic drugs are sometimes disposed of down drains. Amongst other active compounds used, antibiotics and disinfectants are present in the effluent of hospitals (kummerer, 2001). Ciprofloxacin, for example, was found in concentrations of between 0.7 and 124.5mg/L in hospital effluent and was assumed to be the main source of genotoxic effects in hospital effluent (Hartmann et at., 1998). Ampicillin was found in concentrations of between 20 and 80 mg/L in the effluent of a large German hospital. Concentrations as high as 5 mg/L were found for benzalkonium chloride, a quaternary ammonium compound, in the effluent of European hospitals (Kummerer, 2004). Resistant bacteria may be selected or favoured by antibiotic substances in hospital effluent. For single compounds, concentrations calculated and measured in hospital effluents are below MIC values. They may reach this range or even exceed MIC value in hospital effluent if not only single compounds but groups of compounds acting via the same mechanism are considered (Kummerer and Henninger, 2004). Schwartz et al. (2003) found bacteria carrying vanA genes in hospital effluent. The mecA gene encoding resistance against methicillin in staphylococci was only found in bacteria in hospital waste water, but not in bacteria in municipal waste water. Gentamicin resistance genes were found in Acinetobacter, Pseudomonas and Enterobacteriaceae in hospital sewage (Heuer et al. 2002). An important source of the resistance in hospital effluents is also the input of bacteria already resistant because of the use of antibiotics in medical treatment. At present, no data are available for hospital effluents (Kummerer, 2004).
Input of resistant bacteria into municipal sewage.
It is often assumed that hospitals are the most important source for the input of resistant bacteria into municipal waste water. The numbers of resistant bacteria found in the effluent of an intensive care unit (ICU) of a hospital with maximum medical service spectrum were in the same range as those found for the influent of municipal STPs (Kummerer, 2004). Reinthaler and co-workers investigated the resistance of E. coli in three Austrian sewage treatment plants against 24 antibiotics by classical means, i.e. isolation, cultivation and resistance testing. E. coli were resistant to several antibiotics such as penicillins (ampicillin, piperacillin), cephalosporins (cefalothin, cefuroxime), quinolones (nalidixic acid), tetracyclin and sulfamethoxazole/trimethoprim. Resistance rates were highest for tetracyclin (57%) (Reinthaler et al 2003). Resistant and multi-resistant pathogenic bacteria such as Acinetobacter spp. have been detected in waste water and STPs as well as transfer of resistance. Exchange of genes encoding for resistance between pseudomonas and E. coli in sewage sludge has been reported (Schwartz et al., 2003).
Surface water
Concentrations of antibiotics in surface waters, i.e. in rivers and lakes, are in the low microgram per liter range for most compounds. In a study using ciprofloxacin and ceftazidime, it was concluded that the average concentrations of these compounds actually found in surface water will be clearly below concentrations able to change bacterial populations (Wiethan et al., 2000). Bacteria resistant to antibiotics are present in surface water (Muela et al., 1994). Goni-Urizza et al., (2000) found a correlation between resistant bacteria in rivers and urban water input.
Ground water
Antibiotics are rarely found in ground water and if they do occur, they are far below the microgram per liter range. Leaching from fields fertilized with animal slurry or passing through sediments into the ground water might be a source of antibiotics in ground water (Kummerer, 2004).
Drinking water
Antibiotic-resistant bacteria were detected in drinking water as early as the 1948s and later in the 1990s (kummerer, 2004).
Sediments
Resistant bacteria may be present because of the application of antibiotics in fish or because of selection by the antibiotics present in sediments. High antibiotic load in sediments in concentrations sufficiently potent to inhibit the growth of bacteria were reported for aquaculture. Quinolones, sulphonamides and tetracyclines are sorbed by organic matter. Therefore they can accumulate. Bacteria resistant against these compounds have been detected in sediments. (Anderson and Sandaa, 1994; Samuelson et al, 1992) for example, isolated tetracycline- resistant Gram-negative bacteria from polluted and unpolluted marine sediments.
Factors responsible for antimicrobial resistance
Antibiotic use provides selective pressure favoring resistant bacterial strains; inappropriate use by healthcare providers or by way of self-prescribing increase the risk for selection and dissemination of antibiotic-resistant bacteria, which is common in rural Bangladesh and other developing countries (Hossain et al., 1998; Sack et al; 1997; Hoge et al., 1998). These factors, coupled with the overcrowding, poor hygienic practices prevalent in rural people of low socio-economic status, and an increasingly mobile population might have contributed to facilitate the dissemination of antibiotic resistance determinants among the pathogens. Moreover, in developing countries, healthy people commonly harbor resistance bacteria as part of their normal flora and this resistance can be transferred at low frequency via various mechanisms (Hossain et al., 1994).
Lack of education
The combination of poverty and ignorance makes the ground perfect for resistance development. Important reason for irrational therapy is inability to buy adequate quantity of antibiotics or to reach to qualified doctors due to poverty or ignorance for rational prescriptions of antibiotics (Kunin, 1981).
Self-medication with antimicrobials
In many developing countries, antimicrobials are purchased in single doses and taken only until the patient feels better, which may occur before the pathogen has been eliminated (WHO, 1998). In rural Bangladesh, 95% of drugs consumed for 1 month by more than 2000 study participants were suggested by local pharmacies; only 8% were prescribed by physicians (Hossain et al., 1982).
Hospital acquired infections
Hospitals are the places where the selective pressure of antibiotics is the highest as the hospital bacteria are mostly multi drug resistant (Kapil, 1998). The main reason for this is the increase in hospital associated infections because of the disregard to standard isolation precautions in most of the busy hospitals with limited resources (Kaplan et al., 1990) and inappropriate waste disposal.
Use of antibiotics in agriculture or aquaculture
Antibiotics are used widely in agriculture and aquaculture for therapeutic, prophylactic and growth promoting purposes (Gustafson and Bowen, 1997; Willis et al., 1999). The presence of residual antibiotics in the flesh of animals may result in direct exposure of the consumers to these drugs. In addition, the presence of low levels of antibiotics may select for resistant bacteria in the intestines of animals intended for human consumption. The animals can be contaminated with fecal bacteria during the slaughter process and therefore contaminate the meat reaching the consumer. Emergence of VRE (vancomycin resistant enterococci) is one particular example of appearance of resistant bacteria in animals that have affected susceptible human populations (Willis, 2000). Antibiotics resistant bacteria can also be found on fruits and vegetables due to spreading of sewage sludge on farm land or use of antibiotics directly on fruit and vegetable crops (Gustafson and Bowen, 1997).
Environmental factors
The presence of antibiotic resistant bacteria in fresh water sources has been documented from different parts of the world (Willis et al., 1999). Selection of resistant organism in nature may result from the natural production of antibiotics by soil organisms, or contamination from animal feed or crops or waste products from treated animals or humans. Resistant organisms from farming practices may be transferred into rivers and other water sources through waste disposal system or by drainage or rain water from farm land (Gustafson and Bowen, 1997). All these factors contribute to the natural reservoirs of resistance genes which may provide a source of transferable genes.
Use in household products.
There is an increase in the use of surface antibacterial agents over the years into healthy households. The antibacterial substances added to diverse household cleaning products are similar to antibiotics in many ways (Levy, 2001). These products can also select out resistant strains.
Poor quality of antibiotics
During distribution in tropical countries, conditions of transport and storage are poorly controlled, and the drugs may be degraded (Ballereau et al., 1995). Some pharmacologically active drugs produced in industrialized countries have expired when distributed developing countries-they were shipped at the end of the drugs’ shelf lives or their clearance and distribution after transcontinental shipment were delayed (Ballereau et al., 1995).
Emergence of antibiotic resistance in bacteria as an environmental problem
The use of antibiotics and spread of antibiotic resistance in clinical settings is a well recognized problem, but antibiotics and antibiotic resistance as environmental problems and pollutants have largely been overlooked. This is probably due to the fact that antibiotics in non-clinical settings are generally found in concentrations well below those used therapeutically (Jorgensen and Halling-Sorensen, 2000; Kim and Aga, 2007; Rooklidge, 2004). However, even low levels can sustain and/or favor development and spread of antibiotic resistance in microbial communities. It is also important to realize that antibiotics and antibiotic resistance are naturally occurring and play a vital role as regulatory factors in all microbial ecosystems. In addition, several of the antibiotic resistance determinants have primary physiological roles other than giving resistance.
The antibiotics are dispersed in two ways, (1) urine and feces, or (2) direct disposal. A substantial part of all antibiotics consumed are not absorbed or metabolized by the body, but excreted in their active form in the urine and feces. The urine and feces are transported to wastewater treatment plants or can be used directly as manure. Direct disposal includes addition of food additives directly to the water in fish farms or treatment of crops. One large source is probably the disposal of outdated or remainders of antibiotics in household and farm drains (Kummerer, al-Ahmad and Mersch- sundermann, 2000).
Aim of the present study
Escherichia coli related urinary tract infection (UTI), Shigella based dysentery, and Neisseria gonorrhoeae causing gonorrhoea and Staphylococcus aureus related infections are the common infectious diseases and major public health problem in different part of the world as well as in many developing countries like Bangladesh. Due to these diseases there is high death rate among all groups of peoples in Bangladesh. According to survey in 1996 showed that approximately 10-15 thousand patients are dies every year in Bangladesh from urinary tract infection (UTI) due to Escherichia coli. chloramphenicol, a broad-spectrum antibiotic is active against bacteria and other microorganisms, such as rickettsiae. This drug is either bactericidal or bacteriostatic, depending on the microorganisms. The drug has also been reported as alternative medicine in outbreaks caused by multiple resistant Escherichia strain. But in many cases, chloramphenicol is not so effective due to development of resistance and now there is an urgent need to design and identify suitable alternative drug, which will be more effective. In Bangladesh shigellosis is also one of the serious health problems. cotrimoxazole, nalidixic acid is prescribed by the physician as superior drug for the treatment of Shigella infection. This drug has also been reported as alternative medicine in out breaks caused by multi drug resistant Shigella strain. But in many cases cotrimoxazole is not so effective due to development of resistant. In Bangladesh gonorrhoea also possesses severe problems. In fact in this country male who comes with a frankly prurient urethral discharge should be considered as a gonococcal urethetis unless otherwise proved. In recent years the disease appears to have staged a came back with a bang in many advanced countries, where a few decades back, the disease showed a decline in its incidence. This resurgence is probably due to emergence of resistant strains of gonococci and also perhaps due to increasing promiscuity in permissive societies in those countries. Staphylococcus aureus is an important pathogen, which is responsible for a great variety of pyogenic infections in man and animals. The Staphylococci appears to become drug resistant more readily than most other bacteria. In Bangladesh reports on strains resistant to cotrimoxazole, cephranine, erythromycin, gentamycin, ampicillin, chloraphenicol and nitrofuration was documented in a recent investigation.
Drug resistant strains of the above mentioned diseases are developing day by day in our country. Drug resistant may be developed due to irregular intake of antibiotics. Peoples are not so conscious about antibiotic doses. Affected people do not properly follow the treatment procedure of the physician. Therefore, in many cases antibiotics are not so effective due to development of drug resistant strains. So it is our very important and utmost duty to design and identify suitable and effective drug which will be more effective in suppressing the above mentioned diseases. The main aim of this work to characterized the state of resistant pattern of different pathogenic bacteria. The data could be used as means of guidelines for ensuring better treatment for the people of our country. The result of the research will help us to develop and elucidate new and more effective medicine for these deadly bacteria.
Method
Place of research
The research activities of this programme were operated in the laboratory of Microbiology and Industrial Irradiation Division, Institute of Food and Radiation Biology (IFRB), Atomic Energy Research Establishment (AERE), savar, Dhaka.
Source of Strains
Urine which are suspected to contain strains of Staphylococcus aureus, Aerococcus viridans, Moraxella lacunata, Psudomonas diminuta, Listeria monocytogenes collected from the patient in the Gonoshasthaya hospital in savar
Collection of specimens
Urine
‘Midstream’ clean specimens of urine in a sterile container were collected from patient suffering from UTI. Anogenital region was cleaned with antiseptics such as chlorhexidine or cetrimide. The patient then passed urine with labia separated and midstream was collected .Specimens from adult patients were collected carefully in a sterile test tube. Specimens were forwarded to the laboratory as early as possible.
Microbiological analysis of the samples
Analyses were done according to Bergey’s Manual of Determinative Bacteriology (8th edition, 1984).
Media used for microbial study were as follws :
Nutrient agar (NA) media for viable bacterial count.
MacConkey agar media for total coliform count.
The above stated analyses were performed according to the following steps:
Sterilization of glassware
The glassware that are used at microbiological analysis was sterilized by a hot air oven (Memmart, Model TV 10-8042407, Germany) at 1800c for two hours.
Preparation of media
All the above mentioned media were prepared separately by mixing in different conical flask with desired amount of distilled water having appropriate of ingredients that constitute the media .Then the conical flask was sealed with cotton plug and aluminum foil for sterilization .PH of the liquid media ,solution ,etc. was measured by using a TDA PH meter (Model-HM-10K, japan).
Sterilization of media and solution
In an autoclave (Gallenkamp, Model-APP No-713-105 3F, England) under 15 lbs. pressure for 15 minutes at 1210c temperature, media and solution used for the study were sterilized.
Inoculation of media
From each sample one loopful was streaked on nutrient Agar and MacConkey Agar plate. The whole operation was done aseptically no a laminar air bench.
Incubation of media
The nutrient agar plates, MacConkey agar plates were incubated at 370C for 24-48 hours.
Isolation and identification of bacterial strains
To identify the bacterial strains associated with urine samples, the following procedures are follows
Isolation of bacterial strains
Plates with discrete colonies were selected for isolation. Morphologically dissimilar isolated colonies were picked up from plates with the help of sterile loop and each individual colony was streaked on agar plate for pure culture.
Streaking to obtain-single colony isolates (Sharp &Lyles, 1969)
For the isolation of single colony nutrient agar was used .The nutrient agar media was dried and then initial streaking was done with sterile loop using the prepared sample. Then the loop was flamed and next set of streaks were made 3rd set of streaks was made following the same procedure. In every case, flamed loop was partially cooled and allowed to cross on the last streaks (a single time before commencing the next area). The isolated plates were incubated at 370C for 24 hours. After incubation, several colonies were found to grow on isolated condition.
Cultural characteristic
The selected colonies were marked and their cultural characteristic such as shape, size, form, texture, opacity, pigment formation, etc. were observed using hand lens and intensive light then they were recorded.
Purification and preservation of the selected isolates
The selected isolates were then purified through repeated streaked plating .When plating produced only one type of colony in a particular plate, it was considered to be pure .The purified isolates were then transferred to nutrient agar slant in a screw capped culture vial and preserved as stock culture.
Glycerol broth was used for long term preservation of pure culture. A portion of a colony of purified isolates or a loopful of broth culture was densely streaked over the entire surface of PCA plates. The plate was incubated over night at 370C temperature. From the heavy growth area, cells were collected by scraping with a sterile loop. Cells were then suspended thoroughly in glycerol (15%) broth contained in 3 ml screw cap vials. Vilas were then stored at -200C. For the use of the bacteria from the stock culture, the broth first thawed quick just before use. Then one loopful was streaked on fresh PCA plates and incubated over night at 370C. After growing, single colony was collected and transferred to 3ml tryptic soy broth and incubated and used for further biochemical test.
Morphological studies for the identification of the selected strains
With view to identify the selected strains, the following morphological characteristics were studied carefully.
Agar colony
The cultural characteristics of pure isolates on plating agar media were studied after 24 hours or 48 hours incubation carefully. The shape, size, opacity, edge, elevation of the isolated colonies were observed using hand lens and intensive light and were recorded.
Microscopic examination
For all microscopic examination, the slide were scrupulously cleaned and dried for having a good staining. The following techniques were employed for microscopic examination of bacterial strains.
Preparation of smear
Bacteria were grown on Nutrient agar plate at 370C for 24 hours or more according to the necessity. A portion of bacterial culture was taken out by a sterile loop and suspended in sterile normal saline water (0.9% Nacl) solution. This suspension was made sufficiently dilute. A drop of suspension was taken on the slide and a very thin film was made which was allowed to dry in air. This method was followed for almost all type of staining.
Fixation of smear
The smear was fixed by slightly heating the slide over the gas flame. The slide was allowed to be cool before staining.
Staining
The following staining were used on the smear:
Gram staining
1-2 drops of distilled water were placed on a clean slide .Microorganisms were added on it by sterile needle and fixed smear was prepared on the slide .1-2 drops of crystal violet solution was added and keep it for 1 minute. Then the slide was washed with tap water and 1-2 drops of iodine solution was added and kept it for another 1 minute. The slide was then washed with tap water. After those 3-4 drops of ethanol was added on the slide and kept it for 5-7 seconds. Then 1-2 drops of 1% safranin solution were added and kept it for 1 minute. The slide washed with tape water, dried with blotting paper and finally observed under microscope. The presence of crystal violet color indicated the gram-positive and safranin color indicated the gram-negative organisms.
Biochemical characterization
The biochemical tests were performed to confirm the identity of the test organisms are as follows.
(a) Catalase test
Few drops of 24-48 hours tryptic soy broth culture of the test organism were placed in a glass slide. Then few drops of 3% hydrogen peroxide (3% H2O2) solution were added into the drops of the test organism in the slide. The production of bubbles indicates the positive catalase test i.e. catalase producing bacteria.
(b) Indole test
This test was done to determine the ability of the organism to break the amino acid tryptophan to indole. Screw capped tubes containing 5 ml of sterilized tryptic soy broth were inoculated with a loopful of 24-48 hours old culture of the test organisms and incubated for 24 hours at 37˚C temperature. After incubation, 0.5 ml of Kovac’s reagent (p-dimethylaminobenzaldehyde, conc. HCL, isoamyl alcohol) was added and shaken vigorously and wait for sometimes. Kovac’s reagent reacts with the indole and produces a bright red compound on the surface of the medium which indicate the positive indole test.
(c) Voges-Proskaur (VP) test
This test determines the acid producing bacteria. VP medium was inoculated with 24-48 hours old tryptic soy broth culture of the test organism and incubated at 37˚C temperature for 24 to 48 hours. After growth, wearing disposable gloves, o.6 ml of Barritt’s solution A (5% a-naphthol) was added to each of the test tubes followed by 0.2 ml of solution B (40% KOH). Then the tubes were shaken vigorously for 2 minutes. Development of a red color in the medium 15 minutes after following the addition of Barritt’s reagent represents a positive VP test.
(d) Methyl Red (MR) test
The VP medium was also used for the methyl red test. VP medium was inoculated with 24-48 hours old tryptic soy broth cultures of the test organism and incubated at 37˚C temperature for 24 to 48 hours. After incubation a few drops of methyl red solution were added in each test tube. A distinct red color indicated methyl red positive.
(e) Citrate utilization test
This test was done to determine the ability of bacteria to utilize citrate as sole source of carbon for metabolism. Simmon’s citrate agar slants were inoculated with 24-48 hours old tryptic soy broth cultures of the test organism and incubated at 37˚C temperature for 24 to 48 hours. The color change of the medium from green to blue indicates a positive result.
(f) H2S production test
This test was done to determine the ability of bacteria to hydrolyze sulfur containing amino acids such as cysteine. Cysteine, in the presence of cysteine desulfurase, loses its sulfur atom through the addition of hydrogen from water to form H2S gas. SIM (sulfide-indole-motility) agar deeps were inoculated with 24-48 hours old tryptic soy broth cultures of the test organism and incubated at 37˚C temperature for 24 to 48 hours. After growth, all the tubes were examined for the presence or absence of a black color. A black precipitate of FeS indicates the presence of H2S.
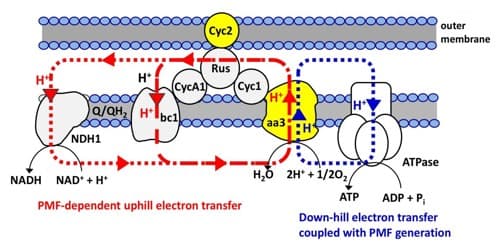
(g) Oxidase test
The ability of bacteria to produce cytochrome oxidase can be determined by the oxidase test. Cytochrome oxidase (aa3 type) uses O2 as an electron acceptor during the oxidation of reduced cytochrome C to form water and oxidized cytochrome C. Tryptic soy agar plates were inoculated with fresh 24 hours old tryptic soy broth cultures of the test organism and incubated at 37˚C temperature for 24 to 47 hours. After taking single colony by a wooden applicator from the plate to a filter paper, a few drops of the oxidase reagent (tetramethyl-p-phenylenediamine dihydrochloride) were added to the colony placed on the filter paper. If the color change to purple or blue is evident within 20 seconds, then the result is positive for oxidase test.
(h) Urease test
This test was done to determine the ability of a bacterium to produce and enzyme called urease that attacks the nitrogen and carbon bond in amide compounds such as urea, forming the end products ammonia, CO2 and water. MIU (Motility-Indole-Ureas) broth tubes were inoculated with 24 to 48 hours old tryptic soy agar slant cultures of the test organism and incubated at 35˚C temperature for 24 to 48 hours. The MIU medium contains the pH indicator phenol red. After growth when the urea was hydrolyzed, ammonia accumulated in the medium and makes it alkaline. This increase in pH causes the indicator to change from orange-red to deep pink or purple. This indicates the positive test result of urease test.
(i) Triple Sugar Iron (TSI) agar test
This test was done to find out the ability of a bacterium to catabolize glucose, lactose, or sucrose and to liberate sulfides from ferrous ammonium sulfate or sodium thiosulfate. Triple sugar iron agar slants were inoculated with 24 to 48 hours old tryptic soy broth cultures of the test organisms by streaking the slant surface using a zigzag streak pattern and then stabbing the agar deep with a straight inoculating needle. The slant tubes were then incubated for 24 to 48 hours in order to detect the presence of sugar fermentation, gas production, and H2S production. The following reactions were occurred in the TSI tubes:
- Yellow butt (A) & red slant (K) due to the fermentation of glucose. Phenol red
Indicator turns yellow due to the persisting acid formation in the butt. The slant remains red (alkaline) because of the limited glucose use in the medium and therefore, limited acid formation, which does not persist.
- Yellow butt (A) & slant (A) due to the fermentation of lactose and/or sucrose leading to excessive acid formation in the entire medium.
- Gas formation noted by splitting of the agar.
- Gas formation (H2S) seen by blacking of the agar.
- Red butt (K) & slant (K) indicates that none of the sugars were fermented and neither gas nor H2S were produced.
(j) Nitrate Reduction test
This test was performed to determine the ability of certain bacteria to reduce nitrate (NO2+) or beyond the nitrate stage .Screw caped tubes containing 10ml of sterilized nitrate broth medium were inoculated with loopful of 24-48 hours old culture of the test organisms and incubated for 24 hours at 370c temperature .After incubation of the culture an organisms ability to reduce nitrates to nitrites is determined by the addition of two reagents. Solution A, which is sulfanilic acid, followed by solution B, which is alpha-naphthylamine. The addition of solution A and B will produce an immediate cherry-red colour which indicates the positive result.
(k) Lysine decarboxylase test
This test was done to find out the ability of a bacterium to decarboxylate lysine. In this test, lysine iron agar was used for the differentiation of enteric organisms based on their ability to decarboxylate or deaminates lysine. Lysine iron agar slants were inoculated with 24 to 48 hours old tryptic soy broth cultures of the test organisms by streaking the slant surface using a zigzag streak pattern and then stabbing the agar deep with a straight inoculating needle. The slant tubes were then incubated with loosened caps for 18-48 hours at 35˚C in an aerobic atmosphere. Lysine decarboxylation was detected in the butt by an alkaline (purple) reaction. Lysine deamination was detected by a red slant.
(l) Gelatin hydrolysis
This test was performed to determine the ability of certain bacteria to producing a proteolytic extracellular emzyme called gelatinase .Screw caped tubes containing 10 ml of sterilized nutrient gelatin were inoculated with loopful of 24-48 hours old culture of the test organisms and incubated for 24 hours at 370c temperature .After incubation, the cultures are placed in refrigerator at 40c for 30 minutes .Cultures that remain liquelied produce gelatinase and demonstrate gelatin hydrolysis which indicate positive gelatin hydrolysis test.
(m) Starch hydrolysis
Organisms capable of hydrolyzing starch to maltose possess the enzyme amylase .By this test the presence or absence of this enzyme in the organisms was ascertained. For this test, starch agar plates were inoculated by streak method and plates were incubated for 72 hours. After growth iodine solution was added to each of the plates. Development of a blue color indicated that starch has not been hydrolysed. Complete hydrolysis and the partial hydrolysis of starch were indicated by the development of clear whitish and bluish or brownish color respectively.
(n) Carbohydrate fermentation test
Fermentation test is one of great significance of in the identification and classification of bacteria. The microorganisms differ in their ability to ferment different carbohydrates .Some of the bacteria produce both acid and carbohydrate fermentation while other produce acid only without gas remaining lots of bacteria cannot ferment carbohydrates.
In this study, the fermentation test of the following carbohydrates and sugar alcohols were done –
1. Pentose : Arabinose, Xylose
2. Mehtyl pentose : Rhamnose
3. Hexoses : Fructose, Galactose, Glucose, Mannose
4. Disaccharides : Cellobiose, Lactose, Maltose, Sucrose
5. Trisaccharide : Raffinose
6. Glycoside : Salicin
7. Alcohols : Adonitol, Dulcitol, Glycerol, Manitol, Sorbitol
8. Non-carbohydrate : Inositol
For carbohydrate fermentation test, first, phenol red carbohydrate broth was prepared and then 1% solution of different carbohydrate was added in different conical flask .In this solution, phenol red was used as indicator. 5 ml of solution was taken in per tube and sterilized in autoclave at 1210C under 15 lbs for 15 minutes. Then the test organisms were inoculated and incubated at 370C for 24 hours t0 48 hours. Positive result was indicated by the change of color from purple to red or yellow.
Drug sensitivity test by disc diffusion method
Antibiotic discs of different concentration were purchase from market and this was placed on a plate of sensitivity testing agar uniformly inoculated with the test organism. The antimicrobials diffused from the disc into the medium and the growth of the test organism is inhibited at a distance from the disc that was related to the sensitivity of the organism. Strains sensitive to the antimicrobial were inhibited at a distance from the disc whereas resistant strains showed smaller zones of inhibition or grow up to edge of the disc.
Anti-microbial discs
The choice of antimicrobials to be inoculated in sensitivity tests will depend on the pathogen, the specimen, range of locally available antimicrobials, and local prescribing policies. Consultation between laboratory, medical, and pharmacy staff was done. By considering these factors for this study, the following antimicrobial discs were used amoxicillin, ampicillin, cephalexim, ciprofloxacin, nalidixic acid, gentamycin, cotrimoxazole and tetracyclin.
Identification of antibiotic resistance
The antibiotics to which specific bacterial strains are resistant were identified by using the disc diffusion method. A 16 hours culture of the strains grown at 37˚C and were spread on a Mueller Hinton agar plate by using a sterilized glass spreader. The plate was allowed to dry. Then antibiotic discs were placed on the plates. The plates were then incubated at 37˚C for 12-16 hours and the growth of the bacteria was observed. The presence of a clear zone around the disc is the index of sensitivity to that antibiotic. The absence of such a zone or the presence of some colonies within the clear zone around the disc is the index of sensitivity to that antibiotic. The absence of such a zone or the presence of some colonies within the clear zone indicated that the collected strains were resistant to that antibiotic. Finally the resistant antibiotic for specific strains was noted.
Radiation effects on specific microorganisms
For the study of radiation effects on some specific microorganisms, all of the selected organisms one single colony of 24 hours cultures of each strain were inoculated to the nutrient broth .The inoculated broth then incubated for 24 hours at 370c and after incubation the samples were send for irradiation at the dose of 0 kGy (control sample), 0.5 kGy, 1.0 kGy, 1.5 kGy, 2.0 kGy, 2.5 kGy, 3.0 kGy, 3.5 kGy, 4.0 kGy, 4.5 kGy and 5.0 kGy of the gamma rays. After irradiation quantitative analysis of microorganisms of the samples were done by using standard microbiological methods.
Result
In a preliminary experiment bacterial sample (urine) were collected from many patients who were suffering from urinary tract infection, Staphylococcal infection where are other disease mentioned in the abstract for the isolation and identification of different pathogens.
After primary collection, through cultural, morphological and biochemical tests those strains which were found to be Staphylococcus aureus, Aerococcus viridians, Pseudomonas diminuta, Moraxella lacunata, Listeria monocytogenes and salmonella salamae were taken to drug resistance study. It was found that 9 isolates were found to be Staphylococcus aureus, 1 isolate were found to be Aerococcus viridians, 1 isolate were found to be pseudomonas diminuta, 2 isolates were found to be Moraxella lacunata, 4 isolates were found to be Listeria monocytogenes and 3 isolates were found to be Salmonella salamae out of 20 isolates.
Twenty different bacterial colonies were inoculated on nutrient agar plate and were allowed to incubate at 370C for 24-48 hours. After incubation cultural characteristic were determined. Morphological characteristic of isolated bacterial strains were determined by gram-staining and microscopic examination.
DISCUSSION
Urinary tract infection, Staplylococcal infection, Shigellosis and gonorrhoea are major health problems in many parts of the world particularly in the developing countries like Bangladesh. In many developing countries the use of antimicrobial drugs for treating people and animals is unregulated, antibiotics can be purchased in pharmacies, general stores, and even market stalls. In the Rajbari district of Bangladesh, a survey of rural medical practitioners (barefoot doctors) with an average of 11 years experience showed that they each saw on average 280 Patients per month and prescribed antibiotics to 60% of these patients on the basis of symptoms alone. In one month 14950 patient were prescribed antibiotics total of 291500 doses. Only 109500 doses had been dispensed by pharmacies and a further 100000 doses had been dispended without a prescription (K. Islam. 2006).
Thus there is widespread and uncontrolled use of antibiotics and patients often do not take a full course of treatment if they are unable to afford it. Another problem in developing countries is the quality and potency of antimicrobial drugs. In some countries many different antimicrobial drugs are produced locally. In India, for example there are over 80 different brands of the fluoroquinolone, ciprofloxacin. In Vietnam a locally acquired 500 mg capsule of ciprofloxacin costs 400 dong (about 2 pence). The average weight of the capsule is 405 mg with potency equivalent to 20 mg of pure ciprofloxacin. Resistance to antibiotics among bacteria limits the options for successful treatment of infectious diseases and increases the risk for complications with severe infections. Emergence of resistance to antibiotics may limit our opportunities to treat harmful impacts on our ecomomy. Some investigators claim that there is danger to human only if resistant pathogens spread to humans (Phillips et al. 2004, Casewell et al, 2003).
In a preliminary experiment bacterial sample (urine) were collected from many patient who were suffering from urinary tract injection (UTI), staphylococcal infection for the isolation and identification of staphylococcus aureus, Aerococcus viridans, Pseudomonas diminuta, Moraxella lacunata, Listeria monocytogenes, Salmonella salamae respectively. During the course of experiment, 20 bacterial isolates were collected.
After primary collection, through, cultural, morphological and biochemical tests were done. It was found that 9 strains were found to be Staphylococcus aureus, I strain were found to be Aerococcus viridans, I strain were found to be Pseudomonas diminuta, 2 strains were found to be Moraxella lacunata, 4 strains were found to be Listeria monocytogenes, 3 strains were found to be Salmonella salamae out of 20 suspected strains.
8 of 9 Staphylococcus aureus isolates it was observed that to the antibiotic amoxicillin (88%) were resistant. On the other hand 1 Staphylococcus aureus isolate were sensitive to amoxicillin, which were strong sensitivity with a zone of inhibition between 10-15 mm in diameter or more. Similar results (83%) have been reported by K. Islam (2006).
7 of 9 Staphylococcus aureus isolates it was observed that to the antibiotic ampicillin (77.77%) were resistant. On the hand 2 staphylococcus aureus isolates were sensitive to ampicillin. Only 1 isolate (11.11%) were strong sensitivity with a zone of inhibition between 10-15 mm in diameter or more. 1 isolates (11.11%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. Similar results (64%) have been reported by K. Islam (2006).
7 of 9 staphylococcus aureus isolates it was observed that to the antibiotic tetracyclin (77.77%) were resistant. On the other hand 2 staphylococcus aureus were sensitive to tetracyclin. 1 isolate (11.11%) were strong sensitivity with a zone of inhibition between 10-15 mm in diameter or more. 1 isolate (11.11%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. Similar results (86%) have been reported by K. Islam (2006).
4 of 9 staphylococcus aureus isolates it was observed that to the antibiotic cotrimoxazole (44.44%) were resistant. On the other hand 5 Stephylococcns aureus isolates were sensitive to cotrimoxazole. Only 2 isolates (22.22%) were strong sensitivity with a zone of inhibition between 10-15 mm diameter or more. 2 isolates (22.22%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (11.11%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar results (46%) have been reported by K. Islam (2006).
3 of 9 Staphylococcus aureus isolates it was observed that to the antibiotic cephalexim (33.33%) were resistant. On the other hand 6 staphylococcus aureus isolates were sensitive to cephalexim. Only 3 isolates (33.33%) were strong sensitivity with a zone of inhibition between 10-15 mm diameter or more. 2 isolates (22.22%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (11.11%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar results (42%) have been reported by K. Islam (2006).
3 of 9 Staphylococcus aureus isolates it was observed that to the antibiotic nalidixic acid (33.33%) were resistant. On the other hand 5 Staplylococcus aureus isolates were sensitive to nalidixic acid. Only 4 isolates (44.44%) wee strong sensitivity with a zone of inhibition between 10-15 mm in diameter or more. 2 isolates (22.22%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. Similar results (54%) have been reported by K. Islam (2006).
2 of 9 Staphylococcus aureus isolates it was observed that to the antibiotic gentamycin (22.22%) were resistant. On the other hand 7 Staphylococcus aureus isolates were sensitive to gentamycin. Only 4 isolates were (44.44%) were strong sensitive with a zone of inhibition between 10-15 mm diameter or more. 2 isolates (22.22%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (11.11%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar results (28%) have been reported by K. Islam (2006).
1 of 9 Staphylococcus aureus isolates was observed that to the antibiotic ciprofloxacin (11.11%) were resistant. On the other hand 8 Staphyolcoccus aureus isolates were sensitive to ciprofloxacin. Only 6 isolates (66.66%) were strong sensitive with a zone of inhibition between 10-15 mm in diameter or more. 2 isolates (11.11%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. Similar results (8%) have been reported by K. Islam (2006).
1 of 1 Aerococcus viridans isolate it was observed that to the antibiotic amoxicillin (100%) wee resistant.
1 of 1 Aerococcus viridans isolate it was observed that to the antibiotic ampicillin (100%) were resistant.
1 of 1 Aerococcus viridans isolate it was observed that to the antibiotic cephalexim (100%) were resistant.
1 of 1 Aerococcus viridans isolate it was observed that to the antibiotic ciprofloxacin (100%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter.
1 of 1 Aerococcus viridans isolate it was observed that to the antibiotic nalidixic acid (100%) were resistan.
1 of Aerococcus viridans isolate it was observed that to the antibiotic cotrimoxazole (100%) were resistant.
1 of 1 Aeroccccus viridans isolate it was observed that to the antibiotic gentamycin (100%) were resistant.
1 of Aerococcus viridans isolate it was observed that to the antibiotic tetracyclin (100%) were resistant.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic amoxicillin (100%) were resistant. This finding is supported by T. Hossan (2007). He reported the similar result (89%) in the studied samples.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic cephalexim (100%) were resistant. This finding is supported by T. Hossan (2007). He reported the similar result (66%) in the studied samples.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic ciprofloxacin (100%) were resistant. This finding is supported by T. Hossan (2007). He reported the similar result (87%) in the studied samples.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic nalidixic acid (100%) were resistant. This finding is supported by T. Hossan (2007). He reported the similar result (67%) in the studied samples.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic gentamycin (100%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. This finding is supported by T. Hossan (2007). He reported the similar result (88%) in the studied samples.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic tetracyclin (100%) were resistant. This finding is supported by T. Hossan (2007). He reported the result (23%) in the studied samples.
1 of 1 Pseudomonas diminuta isolate it was observed that to the antibiotic cotrimoxazole (100%) were resistant. This finding is supported by T. Hossan (2007). He reported the similar result (46%) in the studied samples.
2 of 2 Moraxella lacunata isolates it was observed that to the antibiotic amoxicillin (100%) were resistant.
1 of 2 Moraxella lacunata isolate it was observed that to the antibiotic ampicillin (50%) were resistant. On the other hand 1 isolate (50%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter.
1 of 2 Moraxella lacunata isolate it was observed that to the antibiotic cephalexin (50%) were resistant. On the other hand 1 isolate (50%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter.
2 of 2 Moraxella lacunata isolates it was observed that to the antibiotic ciprofloxacin (100%) were sensitive. 1 isolate were strong sensitive with a zone of inhibition between 10-15 mm diameter or more. 1 isolate were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter.
1 of 2 Moraxella lacunata isolate it was observed that to the antibiotic nalidixic acid (50%) were resistant. On the other hand 1 isolate (50%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter.
1 of 2 Moraxella lacunata isolate it was observed that to the antibiotic cotrimoxazole (50%) were resistant. On the other hand 1 isolate (50%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter.
1 of 2 Moraxella lacunata isolate it was observed that to the antibiotic gentamycin (50%) were resistant. On the other hand 1 isolate (50%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter.
2 of 2 Moraxella lacunata isolates it was observed that to the antibiotic tetracyclin (100%) were resistant.
4 of 4 Listeria monocytogenes isolates it was observed that to the antibiotic tetracyclin (100%) were resistant. Similar observations (73%) have been reported by K. Islam. (2006).
3 of 4 Listera monocytogenes isolates it was observed that to the antibiotic Amoxicillin (75%) were resistant. On the other hand 1 isolate (25%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. Similar observations (61%) have been reported by K. Islam. (2006).
3 of 4 Listeria monocytogenes isolates it was observed that to the antibiotic ampicillin (75%) were resistant. On the other hand 1 isolate (25%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar observations (60%) have been reported by K. Islam. (2006).
1 of 4 Listeria monocytogenes isolate it was observed that to the antibiotic cephalexim (25%) were resistant. On the other hand 3 isolates were sensitive to cephalexim. Only 1 isolate (33.33%) were strongly sensitive with a zone of inhibition between 10-15 mm diameter or more. 1 isolate (33.33%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar observations (36%) have been reported by K. Islam. (2006).
1 of 4 Listeria monocytogenes isolate it was observed that to the antibiotic nalidixic acid (25%) were resistant. On the other hand 3 isolates were sensitive to nalidixic acid. Only 1 isolate (33.33%) were strongly sensitive with a zone of inhibition between 10-15 mm diameter or more. 2 isolates (66.66%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. Similar observations (31%) have been reported by K. Islam. (2006).
1 of 4 Listeria monocytogenes isolate it was observed that to the antibiotic cotrimoxazole (25%) were resistant. On the other hand 3 isolates were sensitive to cotrimoxazole. Only 2 isolates (66.66%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar observations (34%) have been reported by K. Islam. (2006).
4 of 4 Listeria monocytogenes it was observed that to the antibiotic ciprofloxacin (100%) were sensitive. 2 isolates (50%) were strongly sensitive to ciprofloxacin in which zone of inhibition were between 10-15 mm in diameter. 1 isolate (25%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (25%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar observations (76%) have been reported by K. Islam. (2006).
4 of 4 Listeria monocytogenes isolates it was observed that to the antibiotic gentamycin (100%) were sensitive. 3 isolates (75%) were strongly sensitive in which zone of inhibition were between 10-15 mm in diameter. 1 isolate (25%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. Similar observations (87%) have been reported by K. Islam. (2006).
3 of 3 Salmonella salamae isolates it was observed that to the antibiotic amoxicillin (100%) were resistant. This finding is supported by K. Islam (2006). He reported the similar result (72%) in the studied samples.
2 of 3 Salmonella salamae isolates it was observed that to the antibiotic ampicillin (66.66%) were resistant. On the other hand 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. This finding is supported by K. Islam (2006). He reported the similar result (88%) in the studied samples.
2 ot 3 Salmonella salamae isolates it was observed that to the antibiotic tetracyclin (66.66%) were resistant. On the other hand 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. This finding is supported by K. Islam (2006). He reported the result (28%) in the studied samples.
1 of 3 Salmonella salamae isolate it was observed that to the antibiotic cephalexim (33.33%) were resistant. On the other hand 2 isolates were sensitive to cephalexim. Only 1 isolate (33.33%) were strongly sensitive with a zone of inhibition between 10-15 mm in diameter or more. 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. This finding is supported by K. Islam (2006). He reported the similar result (40%) in the studied samples.
1 of 3 Salmonella salamae isolate it was observed that to the antibiotic nalidixic acid (33.33%) were resistant. On the other hand 2 isolates were sensitive to nalidixic acid. 1 isolate (33.33%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. This finding is supported by K. Islam (2006). He reported the similar result (38%) in the studied samples.
1 of 3 Salmonella salamae isolate it was observed that to the antibiotic cotrimoxazole (33.33%) were resistant. On the other hand 2 isolates were sensitive to cotrimoxazole. 1 isolate (33.33%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 1 isolate (33.33%) were weakly sensitive in which zone of inhibition were between 4-6 mm in diameter. This finding is supported by K. Islam (2006). He reported the similar result (35%) in the studied samples.
1 of 3 Salmonella salamae isolate it was observed that to the antibiotic gentamycin (33.33%) were resistant. On the other hand 2 isolates were sensitive to gentamycin. 2 isolates (66.66%) were strongly sensitive with a zone of inhibition between 10-15 mm in diameter or more. This finding is supported by K. Islam (2006). He reported the similar result (288%) in the studied samples.
3 of 3 Salmonella salamae isolates it was observed that to the antibiotic ciprofloxacin (100%) were sensitive. 1 isolate (33.33%) were moderately sensitive in which zone of inhibition were between 7-9 mm in diameter. 2 isolates (66.66%) were weakly sensitive with a zone of inhibition were between 4-6 mm in diameter. This finding is supported by K. Islam (2006). He reported the similar result (30%) in the studied samples.
Conclusion
In this research we tried to characterize the resistant pattern of six different bacteria. Throughout the research work all the isolated strains were identified by different morphological and biochemical tests and finally antibiotic sensitivity tests were done with disc diffusion techniques. From this research it can be concluted that Staphylococcus aureus show maximum resistance to amoxicillin (88.88%), ampicillin (77.77%) and tetracyclin (77.77%). So these antibiotics should not be prescribed for the staphylococcal infection caused by Staphylococcus aureus. In this case ciprofloxacin, gentamycin, ciphalexim may be selected. Aerococcus viridans showed highest resistant to amoxicillin (100%), ampicillin (100%), cephalexim (100%), nalidixic acid (100%), cotrimoxazole (100%), gentamycin (100%) and tetracyclin (100%). So these antibiotics should not be prescribed for human endocarditis caused by Aerococcus viridans. In this case Ciprofloxacin may be selected.
Pseudomonas diminuta showed highest resistance to amoxicillin (100%), ampicillin (100), cephalexim (100%), ciprofloxacin (100%), nalidixic acid (100%), cotrimoxazole (100%) and tetracyclin. So these antibiotics should not be prescribed for the treatment of sepsis, pneumonia and urinary tract infection caused by Pseudomonas spp. So gentamycin may be selected as effective drug for the treatment of Pseudomonal infection. Moraxella lacunata showed highest resistance to amoxicillin (100%) and tetracyclin (100%). So these antibiotics should not be prescribed for the respiratory tract infection caused by Moraxella lacunata. Ciprofloxacin, ampicillin, cephalexim, nalidixic acid, cotrimoxazole and gentamycin may be selected. Listeria manocytogenes showed maximum resistance to tetracyclin (100%), amoxicillin (75%) and ampicillin (75%). So these antibiotics should not be prescribed for the treatment of meningitis, encephalitis, septicemia, endocarditis, abortion and local purulent lesions caused by Listeria monocytogenes. Ciprofloxacin, gentamycin, cephalexim, nalidixic acid and cotrimoxazole may be selected for the treatment of any other infection caused by Listeria monocytogenes. Salmonella salamae showed highest resistance to amoxicillin (100%), ampicilin (66.66%) and tetracyclin (66.66%). So these antibiotics should not be prescribed for the treatment of enterocolitis, septicemia with metastatic abscesses or any other infection caused by Salmonella salamae. Ciprofloxacin, cephalexim, nalidixic acid, cotrimoxazole and gentamycin may be selected.
It is important to note that as the study period was not much lengthy and also the numbers of samples studies were not sufficient to conclude the actual drug resistant pattern of these bacteria but the data found in this study will surely give a picture of drug resistant.
Further more, due to the limitation of our laboratory facilities, it was not possible to characterize the resistant mechanisms in details. Further research work can be carried out with these resistant strains to find out their generic characteristics to see whether their drug resistance property is plasmid or chromosomal DNA mediated, which could help us to develop and effective antibiotics against these resistant strains.