The production of artificial immune cells to combat cancer is an intriguing and rapidly expanding topic of study and development. Artificial immune cells, also known as CAR-T cells (Chimeric Antigen Receptor T-cells), are created immune cells that are designed to more effectively target and destroy cancer cells.
The use of “CAR-T” cells is proving particularly efficient against some blood malignancies among existing immunotherapies, but only in half of patients. The premature malfunction of these immune cells that have been artificially changed in vitro is one of the key reasons for this.
A team from the Universities of Geneva (UNIGE), Lausanne (UNIL), the Geneva University Hospitals (HUG) and the Vaud University Hospital (CHUV), all part of the Swiss Cancer Center Léman (SCCL), has discovered how to prolong the functionality of CAR-T cells. By inhibiting a very specific metabolic mechanism, the team has succeeded in creating CAR-T cells with enhanced immune memory, capable of fighting tumour cells for much longer. These are very promising results, to be read in the journal Nature.
CAR-T cells must be massively multiplied before they can be administered. But the disease history of the patient, in combination with the amplification process, exhausts the cells: they reach a state of terminal differentiation that precipitates the end of their life cycle without leaving them time to act on the length.’
Mathias Wenes
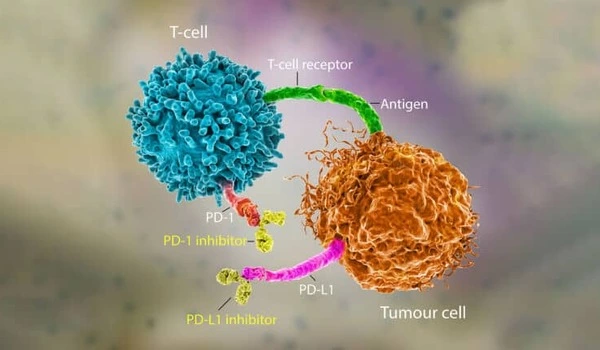
CAR-T cell immunotherapy involves extracting immune cells (typically T lymphocytes) from a cancer patient, altering them in the lab to boost their ability to recognize and destroy tumor cells, and then reinjecting them into the patient. However, as with other types of immunotherapies, many patients fail to react or relapse.
”CAR-T cells must be massively multiplied before they can be administered,” explains Mathias Wenes, a research fellow who coordinated this research in the laboratory of Pr Denis Migliorini, Department of Medicine at the UNIGE Faculty of Medicine and Department of Oncology at HUG. ”But the disease history of the patient, in combination with the amplification process, exhausts the cells: they reach a state of terminal differentiation that precipitates the end of their life cycle without leaving them time to act on the length.”
A mechanism common to cancer cells and immune cells
Cancer cells have a particularly specific survival mechanism in the absence of oxygen: they metabolize the amino acid glutamine as an alternate source of energy via a chemical reaction known as ”reductive carboxylation”. ”Immune cells and cancer cells share a similar metabolism, allowing them to proliferate at a rapid rate. We found that T cells employed this technique as well,” says Alison Jaccard, a Ph.D. student in Professor Ping-Chih Ho’s laboratory at the UNIL-CHUV Department of Oncology and the study’s first author.
To study the significance of reductive carboxylation in CAR-T cells in mice models of leukemia and multiple myeloma, two blood malignancies, the researchers suppressed this pathway in CAR-T cells. ”Our modified CAR-T cells multiplied normally and did not lose their capacity to attack, indicating that reductive carboxylation is not essential for them,” Mathias Wenes sums up.
Mice cured with these CAR-T
Furthermore, the mice treated in this manner were virtually cancer-free, far exceeding the research team’s expectations. ”Without reductive carboxylation, the cells do not differentiate as much and retain their anti-tumor action for a longer period of time. ”They even tend to turn into memory T lymphocytes, a sort of immune cell that preserves the memory of the tumor parts that need to be attacked,” says the researcher.
Memory T lymphocytes play a key role in the secondary immune response. They retain the memory of pathogens previously encountered and can reactivate when they reappear – as in the case of a virus, but also in the case of tumor pathogens – providing much longer-lasting immune protection. ”The same principle applies to CAR-T cells: the higher the number of memory cells, the more effective the anti-tumor response and the better the clinical outcome. The state of differentiation of CAR-T cells is therefore a key factor in the success of the treatment.”
A cross-talk between metabolism and gene expression.
Unfolded, the DNA in each of our cells would be around two meters long. It is condensed around proteins called histones in order to fit into the small cell nucleus. To allow gene transcription to occur, particular DNA sections must unwind, which is accomplished by altering histones. When T cells are activated, histone changes occur that, on the one hand, condense DNA and impede transcription of genes that ensure longevity, while on the other hand open up and allow transcription of genes that drive their inflammatory and killing functions.
Reductive carboxylation influences DNA packing and prevents access to longevity genes by directly affecting the formation of metabolites, which are tiny chemical components that change histones. Its inhibition maintains the opening of those genes and promotes their transformation into long-lived memory CAR-Ts.
















