Inflammation and increased mucus production are common symptoms of worm infections and allergies. This immune response involves our innate immune cells, but their precise functions are unknown. A Charité — Universitätsmedizin Berlin research team has now shed light on the critical tasks that these cells perform. The researchers also identify potential therapeutic approaches for the treatment of allergies in their study, which was published in the journal Nature.
Innate immune cells play a crucial role in protecting the body from infections and other harmful substances. Some of the central functions of innate immune cells include:
Phagocytosis: Innate immune cells, such as neutrophils and macrophages, can engulf and digest pathogens and other foreign particles. This process is called phagocytosis.
Inflammation: Innate immune cells release a variety of inflammatory mediators, such as cytokines and chemokines, which help to recruit other immune cells to the site of infection or injury. This helps to protect the body from further damage and to promote healing.
Antimicrobial activity: Innate immune cells produce a variety of antimicrobial substances, such as lysozyme and defensins, which can kill or inhibit the growth of microorganisms.
Tissue repair: Innate immune cells, particularly macrophages, play a key role in the process of tissue repair by removing dead cells and debris, and by secreting growth factors that stimulate the proliferation and differentiation of new cells.
Regulation of adaptive immunity: Innate immune cells also play a role in regulating the activation and function of adaptive immune cells, such as T cells and B cells. This helps to ensure that the immune response is properly coordinated and that it does not become overactive or inappropriate.
There is a group of adaptive immune cells – namely the T cells – that carry out some similar functions as part of type 2 immune response, so it was previously thought that the role of ILC2s may be redundant and could be easily taken over by the T cells.
Dr. Christoph Klose
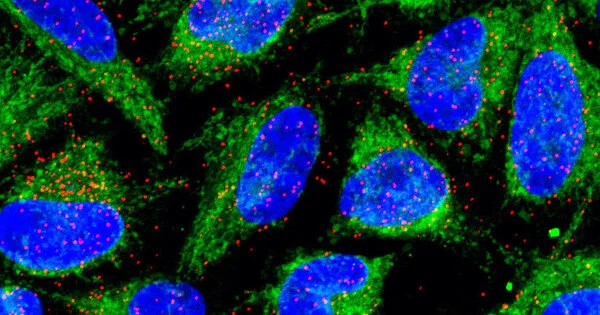
The human immune system is divided into two interconnected branches: the adaptive immune system, which learns something new with each infection and constantly develops over the course of a lifetime, and the innate immune system, which is less specialized but reacts particularly quickly and effectively. The cells of the innate immune system are found in the mucous membranes of the respiratory tract and the intestine, where they serve as the first line of defense against pathogens. These cells include group 2 innate lymphoid cells (ILC2s), which are active in the intestine in the case of parasitic diseases and in the respiratory tract in the case of allergies.
“Innate lymphoid cells were discovered a decade or so ago and we already know a lot about them, but their exact function in the machinery of the immune system is not yet completely understood,” explains Dr. Christoph Klose, who heads the Emmy Noether Independent Junior Research Group on the regulation of type 2 immune responses by neuropeptides and neurotransmitters at the Institute of Microbiology, Infectious Diseases, and Immunology at Charité. “There is a group of adaptive immune cells – namely the T cells – that carry out some similar functions as part of type 2 immune response, so it was previously thought that the role of ILC2s may be redundant and could be easily taken over by the T cells.”
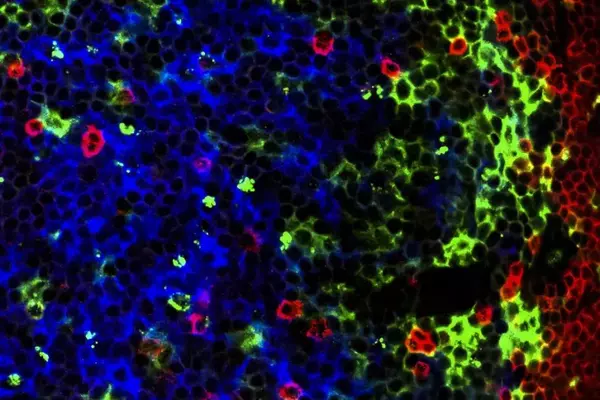
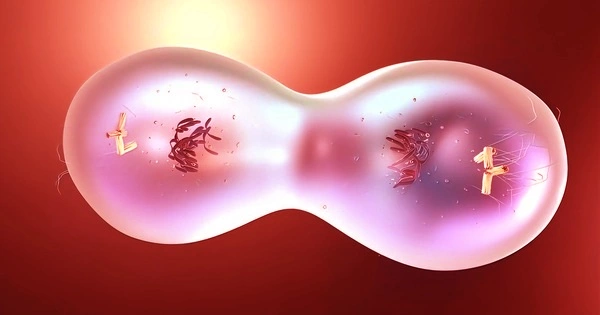
However, the recently published study has now disproved this theory. Using an animal model and state-of-the-art molecular methods such as single-cell sequencing, which allows scientists to zoom into individual cells and analyze their molecular state, they have shed light on the central functions of ILC2s. “A certain type of immune cells called eosinophils were not able to develop properly when ILC2s were absent,” explains Dr. Klose. “This relationship was previously unknown and came as a big surprise.” Eosinophils are involved in inflammatory processes in the tissue.
The scientists also found that ILC2s have a major effect on the ability of epithelial cells to promote mucus production and expel parasites, such as worms, from the body. “The absence of ILC2s was clearly noticeable in our tests examining the immune response to worm infections. There was only limited mucus production in the tissue and the parasites could no longer be combated effectively,” says Dr. Klose, summarizing the results of the study.
In further experiments, the researchers examined the symptoms of allergic asthma and found that these improved when ILC2s were absent. “This could be a starting point for future studies aimed at developing potential allergy therapies,” says Dr. Klose. “With our study, we were able to show that group 2 innate lymphoid cells are essential cogs in the machinery of the immune system and cannot be replaced without compromising the immune response.” In future research projects, Dr. Klose and his team would like to investigate whether innate lymphoid cells regulate other aspects of the immune response.