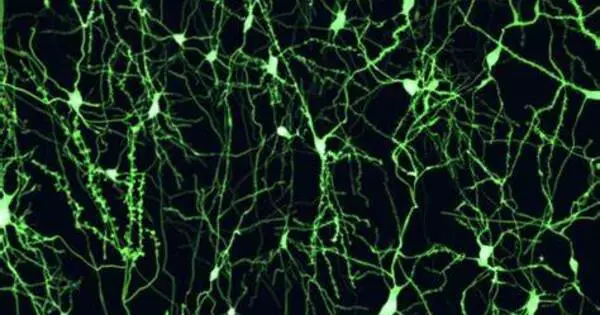
Turning brain immune cells into neurons successfully improves brain function after stroke-like injuries in rats, according to researchers at Kyushu University. These findings, which were published in the journal PNAS on October 10, show that refilling neurons with immune cells could be a potential option for treating stroke in humans.
Stroke and other cerebrovascular illnesses occur when blood flow to the brain is disrupted, resulting in cell damage. Patients frequently have poor recovery, with serious physical limitations and cognitive issues. It is one of the leading causes of long-term care needs worldwide.
“When we get a cut or break a bone, our skin and bone cells can replicate to heal our body. But the neurons in our brain cannot easily regenerate, so the damage is often permanent,” says Professor Kinichi Nakashima, from Kyushu University’s Graduate School of Medical Sciences. “We therefore need to find new ways to replace lost neurons.”
When we get a cut or break a bone, our skin and bone cells can replicate to heal our body. But the neurons in our brain cannot easily regenerate, so the damage is often permanent. We therefore need to find new ways to replace lost neurons.
Professor Kinichi Nakashima
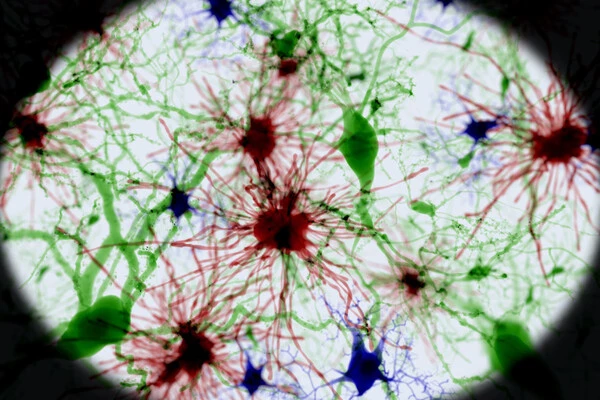
Another option is to transform other brain cells into neurons. The researchers concentrated on microglia, which are the major immune cells in the central nervous system. Microglia are responsible for eliminating damaged or dead cells in the brain, thus after a stroke, they migrate to the site of harm and multiply rapidly.
“Microglia are abundant and precisely where we need them, making them an ideal target for conversion,” explains first author Dr. Takashi Irie of Kyushu University Hospital.
In prior research, the team demonstrated that they could induce microglia to develop into neurons in the brains of healthy mice. Now, Dr. Irie and Professor Nakashima, along with Lecturer Taito Matsuda and Professor Noriko Isobe from Kyushu University Graduate School of Medical Sciences, have shown that this strategy of replacing neurons also works in injured brains and contributes to brain recovery.
The researchers created stroke-like damage in mice by temporarily blocking the right middle cerebral artery, a key blood vessel in the brain that is typically associated with stroke in humans. A week later, the researchers examined the mice and discovered that they had motor function issues as well as a significant loss of neurons in a brain region known as the striatum. This area of the brain is responsible for decision making, action planning, and motor coordination.
The researchers then used a lentivirus to insert DNA into microglial cells at the site of the injury. The DNA held instructions for producing NeuroD1, a protein that induces neuronal conversion. Over the subsequent weeks, the infected cells began developing into neurons and the areas of the brain with neuron loss decreased. By eight weeks, the new induced neurons had successfully integrated into the brain’s circuits.
In behavioral tests three weeks after infection, the mice demonstrated enhanced motor function. When the researchers deleted the newly converted neurons, the benefits were lost, providing strong evidence that the newly converted neurons directly contributed to recovery.
“These findings are quite encouraging. The next step will be to see if NeuroD1 is also effective at converting human microglia into neurons and to confirm that our method of inserting genes into microglial cells is safe,” Professor Nakashima says.
Furthermore, the treatment was carried out in mice during the acute phase of stroke recovery, when microglia were migrating to and replicating at the site of injury. As a result, the researchers intend to test if recovery is possible in mice at a later, chronic stage.