Fatty liver disease, a disorder marked by the buildup of excess fat in the liver, is a major global health concern. Proglucagon-derived peptides (PGDPs), such as glucagon, GLP-1, and GLP-2, are known to influence lipid metabolism in the liver. However, the mechanism behind this remains unknown. Fujita Health University researchers studied the effect of PGDPs, such as glucagon, GLP-1, and GLP-2, in fat storage in the liver using GCGKO mice defective in these peptides.
Fat accumulation in the liver is caused by high-fat diets and obesity, and it is becoming an increasingly serious global health issue. This syndrome, characterized by excessive fat deposition in the liver, increases the risk of developing a variety of metabolic problems. While much of the existing research has focused on fat metabolism within the liver, recent studies highlight the importance of the stomach in this complex process.
Proglucagon-derived peptides (PGDPs), which include glucagon, GLP-1, and GLP-2, are known to be important hormones that control lipid metabolism in the liver. Previous research has demonstrated that GLP-1 and GLP-2, which are derived from the same precursor – proglucagon – play an indirect role in fat buildup in the liver. However, their specific contributions to liver fat accumulation are not yet fully understood.
When we subjected both GCGKO mice and control mice to an HFD for one week, the GCGKO mice exhibited a significantly lower increase in hepatic free fatty acid (FFA) and triglyceride levels, along with reduced adipose tissue weight.
Dr. Seino
A new study, led by Associate Professor Yusuke Seino from Fujita Health University and published in Nutrients, explores how PGDPs impact fat absorption and liver fat buildup. The team of researchers included lead researchers Mr. Koki Nishida, Mr. Atsushi Suzuki, and Mr. Yoshiki Hirooka from Fujita Health University, along with Mr. Yoshikata Hayashi from Nagoya University. Using genetically modified mice lacking PGDPs (GCGKO mice), the study investigates the response of mice to a high-fat diet (HFD) for seven days and sheds light on a potential new strategy for preventing fatty liver.
“When we subjected both GCGKO mice and control mice to an HFD for one week, the GCGKO mice exhibited a significantly lower increase in hepatic free fatty acid (FFA) and triglyceride levels, along with reduced adipose tissue weight,” highlighted Dr. Seino. These effects were attributed to a decrease in lipid absorption via the CD36 pathway in the intestinal tract, despite a reduced fat-burning capacity (β-oxidation) in the liver.
In addition, the study discovered reduced expression levels of genes involved in FFA oxidation in HFD-fed GCGKO mice. Pparα (peroxisome proliferator receptor alpha) and Cd36 (cluster of differentiation 36) mRNA levels decreased in the duodenum, leading to decreased fat uptake and increased fecal cholesterol levels. This shows that PGDP deficiency protects diet-induced fatty liver by reducing intestinal fat absorption.
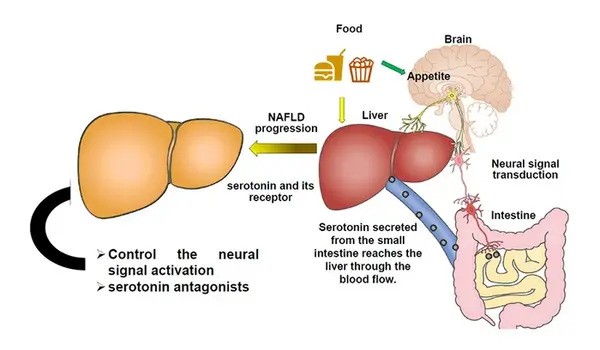
Notably, the researchers discovered that, despite reduced fat-burning activity in the liver, the key determinant limiting fat buildup was decreased fat absorption from the intestines. HFD-fed GCGKO mice had lower plasma triglyceride levels during the oral fat tolerance test (OFTT), confirming reduced lipid absorption.
Furthermore, the study emphasizes the complex link between nutrition, hormonal responses, and the intestinal flora. The HFD-fed GCGKO mice showed significant alterations in gut flora, with an increase in Parabacteroides and a decrease in Lactobacillus, both of which are associated with obesity resistance. These alterations support the feasibility of dietary and hormonal therapies to improve gut health and metabolic function.
Adding further, Dr. Seino notes, “If we can examine in more detail how PGDPs specifically regulate lipid absorption in the gut, we hope to clarify the relationship between diet, hormones, and intestinal bacteria sufficiently to recommend a diet that is less conducive to obesity and fatty liver disease.”
Dr. Seino discusses the long-term ramifications of their findings, saying, “In the future, oral dual antagonists of GLP-2 and glucagon could emerge as potential therapies for obesity and fatty liver, especially given their roles in insulin sensitivity and lipid metabolism.”
In conclusion, our findings pave the path for the development of tailored medicines to tackle this rising health concern, potentially improving outcomes for millions of patients suffering from fatty liver disease globally.