A high dietary fat intake has a significant impact on the risk of acquiring cardiovascular disease (CVD). Saturated fatty acids, which are often present in dairy and meat, boost cholesterol levels. Furthermore, research has revealed that trans fatty acids, which are contained in industrially hardened oils, increase the risk of coronary heart disease. While trans fatty acids have been removed from many spreads around the world, they can still be present in deep-fried fast foods and baked goods.
Macrophages eat fat as they move through our arteries. Fat-filled macrophages, on the other hand, can restrict blood arteries and induce heart disease. In Nature Cardiovascular Research, UConn Health researchers report how eliminating a protein could prevent this and potentially avoid heart attacks and strokes in patients.
Macrophages are enormous white blood cells that act as a sort of clean-up team in our bodies, sweeping out dangerous waste. However, macrophages can cause problems in those who have atherosclerosis, which is characterized by fatty deposits and inflammation in the blood vessels. They consume extra fat within artery walls, but the fat causes them to froth. Furthermore, foamy macrophages promote artery inflammation and can sometimes break off plaques, releasing clots that might cause a heart attack, stroke, or embolism elsewhere in the body.
TRPM2 was removed from a variety of lab mouse that is prone to atherosclerosis. Taking off that protein didn’t seem to harm the mice, and it kept the macrophages from foaming up. It also helped the animals with their atherosclerosis.
Yue and Pengyu Zong
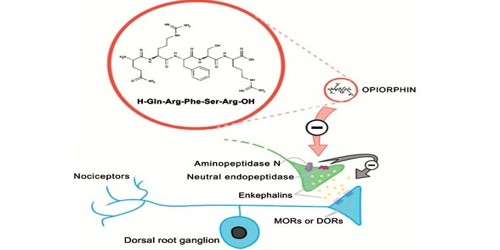
Changing how macrophages express a certain protein could avoid this type of harmful behavior, according to a team of UConn Health researchers. They discovered that inflammation activates the protein known as TRPM2. It instructs macrophages to begin consuming fat. TRPM2 is highly activated because one of the key causes of atherosclerosis is inflammation of the blood arteries. TRPM2 activation stimulates macrophage activity, resulting in more foamy macrophages and potentially more inflamed arteries. According to Lixia Yue, a cell biologist at UConn School of Medicine, the method TRPM2 increased macrophage activity was remarkable.
“They form a vicious cycle promoting the development of atherosclerosis,” Yue says.
Yue and Pengyu Zong, the paper’s lead author and a graduate student, demonstrated one approach to break the loop, at least in mice. TRPM2 was removed from a variety of lab mouse that is prone to atherosclerosis. Taking off that protein didn’t seem to harm the mice, and it kept the macrophages from foaming up. It also helped the animals with their atherosclerosis.
Yue and Pengyu Zong, together with the rest of the team, are now investigating whether elevated TRPM2 expression in blood monocytes (precursors to macrophages) correlates with the severity of cardiovascular disease in patients. If they discover a link, high levels of TRPM2 could be a risk factor for heart attack and stroke.
Although you may be aware that some foods can increase your risk of heart disease, altering your eating habits can be difficult. Whether you’ve been eating improperly for years or you just want to fine-tune your diet, here are eight heart-healthy diet suggestions to get you started. You’ll be on your way to a heart-healthy diet once you know which foods to eat more of and which meals to avoid.
The liver produces cholesterol, which is an essential component of cell membranes and certain hormones, but it is also found in dairy products, meat, and eggs. A high level of a certain form of cholesterol (Low-Density Lipoprotein or LDL) in the blood can cause its accumulation in the arteries, limiting blood flow and potentially causing heart issues. Although it is unclear whether dietary cholesterol is linked to cardiovascular disease, it is advised to limit one’s intake. Cholesterol is not necessary in the diet because it is produced in sufficient quantities by the liver.
High salt (sodium) intake has been related to high blood pressure, which is a major risk factor for stroke and coronary heart disease. There is compelling evidence that reducing daily salt intake (by 50 mmol, or about 1.2g globally) would result in a reduction in the number of fatalities from strokes and coronary heart disease (by about 22 percent and 16 percent respectively).
It has been demonstrated that taking potassium supplements lowers blood pressure and the risk of CVD. However, the recommended level of fruit and vegetable consumption provides an adequate potassium intake, and there is no evidence to support long-term potassium supplementation to reduce the risk of CVD.