Researchers revealed that a mutation in the cellulose-producing machinery of E. coli bacteria allows them to cause serious sickness in humans; ‘good’ bacteria produce cellulose, but ‘bad’ bacteria do not. The alterations prevented E. coli from producing the cell-surface carbohydrate cellulose, which caused greater inflammation in the host’s intestinal tract, culminating in the breakdown of the intestinal barrier, allowing the bacteria to travel throughout the body. Understanding how bacteria move from intestine reservoirs to the rest of the body is critical for preventing infections and combating antibiotic resistance.
Queensland researchers have discovered that a mutation allows some E. coli bacteria to cause severe disease in people while other bacteria are harmless, a finding that could help to combat antibiotic resistance.
Professor Mark Schembri and Dr Nhu Nguyen from The University of Queensland’s Institute for Molecular Bioscience and Associate Professor Sumaira Hasnain from Mater Research found the mutation in the cellulose making machinery of E. coli bacteria.
Professor Schembri said the mutation gives the affected E. coli bacteria the green light to spread further into the body and infect more organs, such as the liver, spleen and brain.
Our discovery explains why some E. coli bacteria can cause life-threatening sepsis, neonatal meningitis and urinary tract infections (UTIs), while other E. coli bacteria can live in our bodies without causing harm.
Professor Schembri
“Our discovery explains why some E. coli bacteria can cause life-threatening sepsis, neonatal meningitis, and urinary tract infections (UTIs), while other E. coli bacteria can live in our bodies without causing harm,” Professor Schembri said.
“The ‘good’ bacteria make cellulose and ‘bad’ bacteria can’t.”
Bacteria produce many substances on their cell surfaces that can stimulate or dampen the immune system of the host.
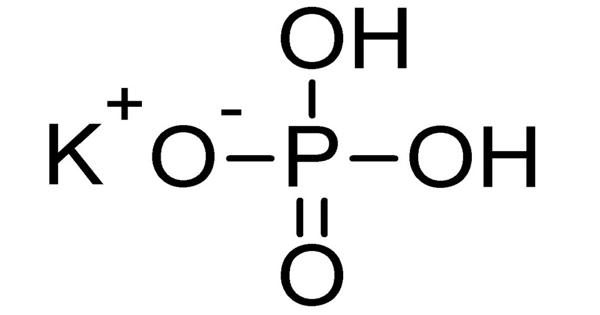
“The mutations we identified stopped the E. coli making the cell-surface carbohydrate cellulose and this led to increased inflammation in the intestinal tract of the host,” Professor Schembri said. “The result was a breakdown of the intestinal barrier, so the bacteria could spread through the body.”

In models that replicate human disease, the team showed that the inability to produce cellulose made the bacteria more virulent, so it caused more severe diseases, including infection of the brain in meningitis and the bladder in UTIs. Associate Professor Hasnain said understanding how bacteria spread from intestinal reservoirs to the rest of the body was important in preventing infections.
“Our finding helps explain why certain types of E. coli become more dangerous and provides an explanation for the emergence of different types of highly virulent and invasive bacteria,” she said.
Professor Schembri said E. coli was the most dominant pathogen associated with bacterial antibiotic resistance.
“In 2019 alone, almost 5 million deaths worldwide were associated with bacterial antibiotic resistance, with E. coli causing more than 800,000 of these deaths,” he added. “As the threat of superbugs that are resistant to all available antibiotics increases worldwide, finding new ways to prevent this infection pathway is critical to reduce the number of human infections.”
The partnership includes teams from the University of Queensland’s School of Biomedical Sciences, led by Associate Professor Jana Vukovic, and Griffith University’s School of Pharmacy and Medical Sciences, directed by Professor Glen Ulett.