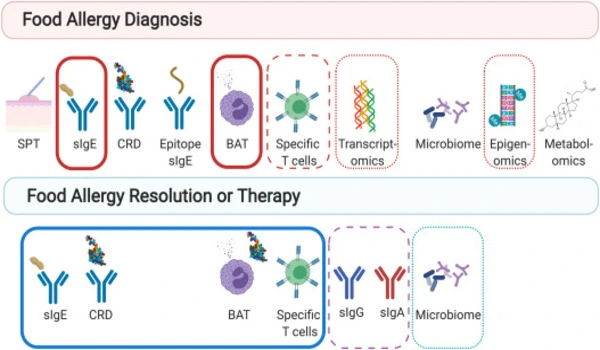
For the first time, researchers from Ann & Robert H. Lurie Children’s Hospital in Chicago and colleagues showed that a genetic biomarker could help predict the severity of food allergy reactions. There is currently no reliable or widely available clinical biomarker that can effectively discriminate between people with food allergies who are at risk for severe life-threatening reactions and those who have milder symptoms. The findings were reported in the journal Allergy and Clinical Immunology.
Lang et al. discovered that individuals with α-tryptase, an enzyme isoform encoded by the TPSAB1 gene, have a higher risk of anaphylaxis or severe food reactions compared to those who do not have it.
Research in this area often aims to understand the genetic factors that contribute to the development and severity of food allergies. Genetic biomarkers, if identified, could potentially help in predicting the likelihood of an individual developing a severe reaction to certain foods.
Determining whether or not a patient with food allergies has α-tryptase can easily be done in clinical practice using a commercially available test to perform genetic sequencing from cheek swabs.
Abigail Lang
“Determining whether or not a patient with food allergies has α-tryptase can easily be done in clinical practice using a commercially available test to perform genetic sequencing from cheek swabs,” said lead author Abigail Lang, MD, MSc, attending physician and researcher at Lurie Children’s and Assistant Professor of Pediatrics at Northwestern University Feinberg School of Medicine.
“If the biomarker is detected, this may help us understand that the child is at a higher risk for a severe reaction or anaphylaxis from their food allergy and should use their epinephrine auto-injector if exposed to the allergen. Our findings also open the door to developing an entirely new treatment strategy for food allergies that would target or block α-tryptase. This is an exciting first step and more research is needed.”
Tryptase is mostly found in mast cells, which are white blood cells that are part of the immune system. Mast cells are triggered during allergic responses. higher TPSAB1 copy number, resulting in higher α-tryptase, has been linked to severe reactions in adults with Hymenoptera venom allergy (or anaphylaxis following a bee sting).
Dr. Lang’s study included 119 participants who underwent TPSAB1 genotyping, 82 from an observational food allergy cohort at the National Institute of Allergy and Infectious Diseases (NIAID) and 37 from a cohort of children who reacted to peanut oral food challenge at Lurie Children’s.
“We need to validate our preliminary findings in a much larger study, but these initial results are promising,” says Dr. Lang. “We also still need a better understanding of why and how α-tryptase makes food allergy reactions more severe in order to pursue this avenue for potential treatment.”