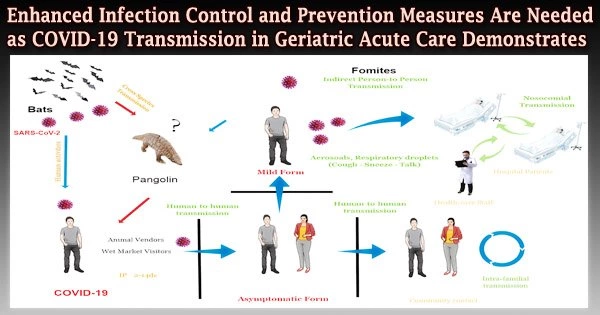
In a study that was just published in eLife, researchers from Switzerland and the UK discovered that there was less virus transmission between patients and healthcare providers in COVID-19 isolation wards than was anticipated.
However, the study discovered that when an outbreak occurred, healthcare workers on other wards tended to be the main source of new hospital-acquired diseases. The results show differences in infection control procedures between various acute care wards.
The majority of COVID-19 deaths reported globally are believed to have been caused by hospital-acquired cases of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in geriatric institutions and long-term care facilities (LTCF).
Regarding the virus’s transmission chains in various settings and the corresponding contributions of patients and healthcare workers, there is still some doubt.
“Because the reservoir of SARS-CoV-2 in healthcare environments may contribute to amplifying the pandemic, we need to better understand transmission dynamics in these settings,” says lead author Mohamed Abbas, Senior Research Associate at the Infection Control Programme, Geneva University Hospitals, Switzerland, and Honorary Clinical Research Fellow at the MRC Centre for Global Infectious Disease Analysis, Imperial College London, UK.
“Detecting and defining cases is crucial in settings with a high patient turnover, or where patients are admitted from the community and both COVID-19 and non-COVID-19 cases are cared for in the same institution. If we can determine the sources of infection and transmission pathways, we can improve infection prevention and control strategies.”
Our study shows transmission dynamics among healthcare workers differ according to whether they worked in COVID-19 wards or wards where outbreaks occurred. This could suggest that those working on COVID-19 wards were concerned about becoming infected and applied infection control measures rigorously, whereas those working on non-COVID wards may have underestimated the risk of transmission.
Professor Stephan Harbarth
The team’s goal was to reassemble the dynamics of transmission in a number of hospital-based COVID-19 outbreaks that involved both patients and medical personnel at the 196 acute-care and 100 rehabilitation beds Swiss university-affiliated Hospital of Geriatrics.
176 acute care beds were set aside in 2020 for COVID-19 patients who didn’t need intensive care during the first wave of the pandemic. Other patients were admitted at the same time for reasons unrelated to COVID-19, and they shared beds for rehabilitation with COVID-19 patients who were recovering from their illness.
The team constructed a mathematical model including data on contact networks between patients and healthcare personnel to examine the transmission between patients and healthcare professionals on these wards.
In an infector/infectee pair, they took into account the intervals between infections as well as a genetic sequence evolution model that demonstrates if one illness has evolved from another. They next contrasted this with the transmission dynamics they anticipated to happen at random among the COVID-19 ward’s medical staff and patients.
Of the 127 SARS-CoV-2 positive cases, 36 were among healthcare staff working in non-COVID-19 wards where outbreaks were place, and 48 patients caught the virus while residing in a ward where an outbreak took place.
Instead of sharing a room, the majority of patient-to-patient transmission occurred among patients who had shared a ward. It was twice as likely than expected for patients in a ward where an outbreak had occurred to contract hospital-acquired COVID-19 from other patients.
Similar to this, healthcare professionals were more than twice as likely to contract the illness from a colleague who worked on a ward where an epidemic had occurred than from one of the COVID-19 units.
The statistics also indicate that healthcare personnel on a ward with an epidemic may have contributed to more COVID-19 secondary cases than hospitalized COVID-19 patients.
“Our study shows transmission dynamics among healthcare workers differ according to whether they worked in COVID-19 wards or wards where outbreaks occurred. This could suggest that those working on COVID-19 wards were concerned about becoming infected and applied infection control measures rigorously, whereas those working on non-COVID wards may have underestimated the risk of transmission,” concludes senior author Stephan Harbarth, Professor of Infectious Diseases at the Infection Control Programme, Geneva University Hospitals.
“Strategies to prevent SARS-CoV-2 transmission in geriatric settings should take into account the potential for patient-to-patient transmission and the transmission dynamics between healthcare workers in non-COVID-19 wards, which may differ considerably from those in dedicated COVID-19 wards.”