People with cancer may try complementary or alternative therapies to help with diet issues or to treat the disease. Alternative diets have not been scientifically proven to cure cancer. Most alternative therapies have not been subjected to such scrutiny. As a result, there is no scientific proof that they work. Some alternative therapies may not be completely risk-free. They may have negative side effects. People frequently use complementary and alternative therapies to feel more in control of their lives. They offer some people hope and psychological support.
A dietary change may be the key to improving colon cancer treatment, according to a new study from the University of Michigan Rogel Cancer Center.
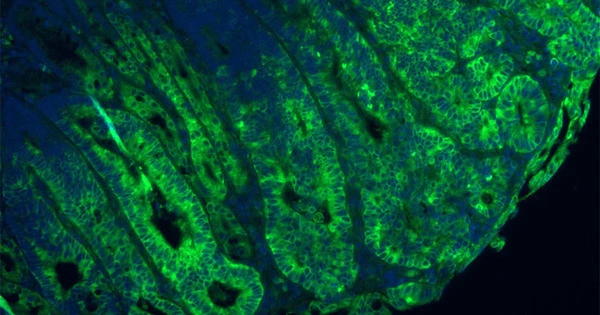
Cancer cells require nutrients in order to survive and grow. mTORC1 is one of the most important nutrient-sensing molecules in a cell. It is often referred to as a master regulator of cell growth because it allows cells to sense different nutrients and thus grow and proliferate. When nutrients are scarce, cells reduce the nutrient-sensing cascade and inhibit mTORC1.
While mTORC1 is known to be hyperactive in colon cancer, the key question is whether tumors use nutrient sensing pathways to activate the master regulator.
We knew that nutrients were important in mTORC regulation but we didn’t know how they directly signal to mTORC. We discovered the nutrient signaling pathway is just as important to regulate mTORC as the oncogenic signaling pathway.
Sumeet Solanki
“When the nutrients available in the tumors are reduced in colon cancer, the cells become confused. Without nutrients to grow, they go through a kind of crisis, which results in massive cell death “Yatrik M. Shah, Ph.D., Horace W. Davenport Collegiate Professor of Physiology at Michigan Medicine, is the study’s senior author.
A low-protein diet, researchers discovered in cells and mice, blocked the nutrient signaling pathway that activates a master regulator of cancer growth. The findings were published in the journal Gastroenterology.
The regulator, mTORC1, controls how cells use nutritional signals to grow and multiply. It’s highly active in cancers with certain mutations and is known to cause cancer to become resistant to standard treatments. A low-protein diet, and specifically a reduction in two key amino acids, changed the nutritional signals through a complex called GATOR.
GATOR1 and GATOR2 work together to keep mTORC1 in business. When a cell has plenty of nutrients, GATOR2 activates mTORC1. When nutrients are low, GATOR1 deactivates mTORC1. Limiting certain amino acids blocks this nutrient signaling.

Previous efforts to block mTORC have focused on inhibiting its cancer-causing signals. But these inhibitors cause significant side effects – and when patients stop taking it, cancer comes back. The study suggests that blocking the nutrient pathway by limiting amino acids through a low-protein diet offers an alternative way to shut down mTORC.
“We knew that nutrients were important in mTORC regulation but we didn’t know how they directly signal to mTORC. We discovered the nutrient signaling pathway is just as important to regulate mTORC as the oncogenic signaling pathway,” said study first author Sumeet Solanki, Ph.D., a research investigator at the Rogel Cancer Center.
Researchers confirmed their findings in cells and mice, where they saw that limiting amino acids stopped cancer from growing and led to increased cell death. They also looked at tissue biopsies from patients with colon cancer, which confirmed high markers of mTORC correlated with more resistance to chemotherapy and worse outcomes. Solanki said this could provide an opportunity to direct treatment for patients with this marker.
“A low-protein diet won’t be standalone treatment. It has to be combined with something else, such as chemotherapy,” Solanki said. The risk with a low-protein diet is that people with cancer often experience muscle weakness and weight loss, which limiting protein could exacerbate.
“Putting cancer patients on a protein-deficient diet long-term is not ideal. But if you can find key windows – like at the start of chemotherapy or radiation – when patients could go on a low protein diet for a week or two, we could potentially increase the efficacy of those treatments,” Shah said.
Further research will refine this concept of a therapeutic window to limiting amino acids. Researchers will also seek to understand how these pathways are creating resistance to treatment and whether an inhibitor could block the GATOR complexes.