Blood clotting abnormalities can be caused by a variety of reasons, such as a genetic predisposition, particular drugs, underlying medical conditions, and lifestyle choices. Adenovirus infection, one of the most prevalent respiratory viruses in pediatric and adult patients, may trigger a life-threatening blood clotting condition, according to new research.
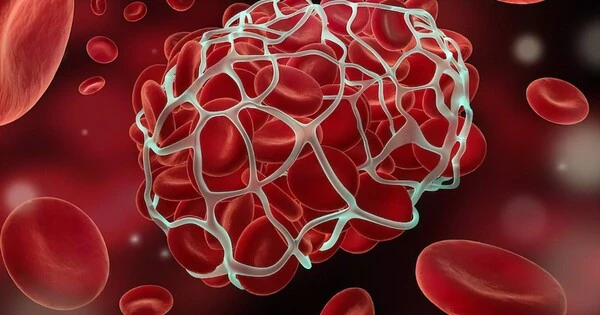
Platelets, also known as thrombocytes, are specialized cellular fragments that produce blood clots in the event of a scrape or traumatic injury. Platelet levels can diminish throughout the body as a result of viral infections, autoimmune disease, and other disorders, a condition known as thrombocytopenia.
Stephan Moll, MD, and Jacquelyn Baskin-Miller, MD, both of the UNC School of Medicine, have connected adenovirus infection to a rare blood clotting condition after a rigorous clinical and research partnership. This is the first time a common respiratory virus that causes moderate cold and flu-like symptoms has been linked to blood clots and severe thrombocytopenia.
“This adenovirus-associated disorder is now one of four recognized anti-PF4 disorders,” said Moll, a professor of medicine in the Division of Hematology at the University of Michigan. “We hope that our findings will lead to earlier diagnosis, more appropriate and optimized treatment, and better outcomes in patients who develop this life-threatening disorder.”
Their new observation, which was published in the New England Journal of Medicine, sheds new light on the virus and its role in causing an anti-platelet factor 4 disorder. Additionally, the discovery opens a whole new door for research, as many questions remain as to how and why this condition occurs – and who is most likely to develop the disorder.
This adenovirus-associated disorder is now one of four recognized anti-PF4 disorders. We hope that our findings will lead to earlier diagnosis, more appropriate and optimized treatment, and better outcomes in patients who develop this life-threatening disorder.
Stephan Moll
HIT, VITT, and “Spontaneous HIT”
Antibodies are large Y-shaped proteins that can stick to the surface of bacteria and other “foreign” substances, flagging them for destruction by the immune system or neutralizing the threat directly.
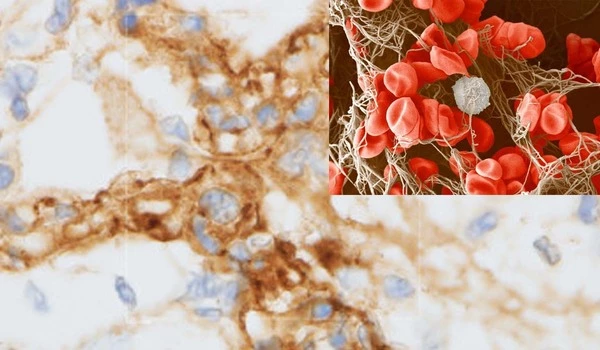
Anti-PF4 diseases are caused by the immune system producing antibodies against platelet factor-4 (PF4), a protein produced by platelets. When an antibody develops and attaches to PF4, it can cause platelets in the bloodstream to be activated and rapidly removed, resulting in blood clotting and depleted platelets.
Anti-PF4 antibody development is sometimes prompted by a patient’s exposure to heparin, which is known as heparin-induced thrombocytopenia (HIT), and occasionally it occurs as an autoimmune illness without heparin exposure, which is known as “spontaneous HIT.”
In the last three years, thrombocytopenia has been shown to rarely occur after injection with COVID-19 vaccines that are made with inactivated pieces of an adeno-viral vector. These vaccines are different than the ones made in the United States, such as those by Moderna and Pfizer. The condition is referred to as vaccine-induced immune thrombotic thrombocytopenia (VITT).
The Road to Discovery
The path to the discovery began when a 5-year-old boy was admitted to the hospital with an aggressive blood clot growing in his brain (called cerebral sinus vein thrombosis) and acute thrombocytopenia after being diagnosed as an outpatient with adenovirus infection. Doctors confirmed that he had not been exposed to heparin or the adeno-vector COVID-19 immunization, both of which are known to be HIT and VITT triggers.
“The intensive care unit physicians, the neuro-intensivist, and hematology group were working around the clock to determine next steps in the care for this young boy,” said Baskin-Miller. “He wasn’t responding to therapy and was progressing quickly. We had questioned whether it could have been linked to his adenovirus considering the vaccine data, but there was nothing in the literature at that time to suggest it.”
The collaborative clinical effort to help the patient expanded: Baskin-Miller reached out to Moll, who is an expert in thrombosis and has various connections throughout the field. To Moll, it looked like the pediatric patient could have “spontaneous HIT.” They then tested for the HIT platelet activating antibody, which came back positive.
Collaboration is Key
Moll reached out to, Theodore E. Warkentin, MD, a professor of pathology and molecular medicine at McMaster University in Hamilton, Ontario, who has been researching anti-PF4 disorders for three decades, to hear if he was aware of an association between adenoviral infection and spontaneous HIT. Warkentin, who is one of the premier international anti-PF-4 disorders researcher, wasn’t aware of the condition.
At around the same time, Moll received a phone call from Alison L. Raybould, MD, a hematologist-oncologist in Richmond, Virginia, and a former UNC trainee. She was seeing a patient who had many blood clots, a stroke and heart attack, deep-vein thromboses (DVT) in both arms and legs, and significant thrombocytopenia.
Heparin and vaccinations had not been administered to the patient. However, this patient’s severe sickness began with viral symptoms such as cough and fever, and she tested positive for adenoviral infection. Anti-PF4 antibody testing revealed a positive result as well.
To further clarify the diagnosis of the two patients, Warkentin quickly offered to analyze their blood, and samples were sent directly to his laboratory at Hamilton General Hospital. They confirmed that the antibodies, like the HIT antibodies, were targeting platelet factor 4.
Surprisingly, the antibody resembled the VITT antibody and attached to PF4 in the same area as the VITT antibody. They came to the conclusion that both patients had “spontaneous HIT” or a VITT-like condition caused by an adenovirus infection.