Bacteria treatment for lowering insulin resistance and preventing diabetes is a topic of active research, with some encouraging results in recent years. The aim behind this method is to use certain types of bacteria, particularly those found in the gut microbiome, to alter metabolic processes in the body.
Researchers at the RIKEN Center for Integrative Medical Sciences (IMS) in Japan, lead by Hiroshi Ohno, have discovered a form of gut bacteria that may help improve insulin resistance and so protect against the development of obesity and type 2 diabetes. The research, which was published on August 30 in the scientific journal Nature, involved genetic and metabolic studies of human fecal microbiomes, followed by corroborating trials in fat mice.
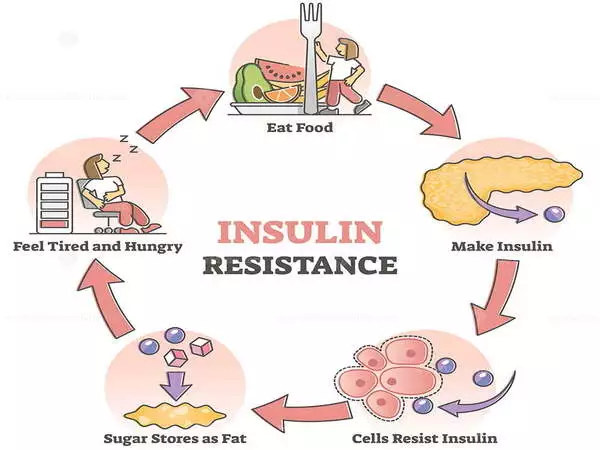
Insulin is a hormone produced by the pancreas in response to high blood sugar levels. Normally, it aids in the transport of sugar into the muscles and liver, allowing them to use the energy. Insulin resistance occurs when insulin is unable to do its function, causing more sugar to remain in the blood and the pancreas to produce more insulin. Insulin resistance can result in obesity, pre-diabetes, and type 2 diabetes.
Trillions of bacteria live in our guts, many of which break down carbohydrates that would otherwise go undigested. While many have argued that this occurrence is linked to obesity and pre-diabetes, the facts remain murky due to the diversity of bacteria and a lack of metabolic data. Ohno and his colleagues at RIKEN IMS addressed this gap with a comprehensive investigation, discovering a type of bacteria that may aid in the reduction of insulin resistance in the process.
We discovered that higher insulin resistance was associated with an abundance of carbohydrates in the feces, particularly monosaccharides like glucose, fructose, galactose, and mannose.
Hiroshi Ohno
First, scientists looked for as many metabolites as they could find in the excrement of over 300 persons during routine health checks. They matched this metabolome to insulin resistance levels measured in the same individuals. “We discovered that higher insulin resistance was associated with an abundance of carbohydrates in the feces,” Ohno explains, “particularly monosaccharides like glucose, fructose, galactose, and mannose.”
They then studied the research participants’ gut flora and its association to insulin resistance and fecal carbohydrates. Bacteria from the taxonomic order Lachnospiraceae were found in greater abundance in the stomachs of persons with higher insulin resistance than bacteria from other orders. Furthermore, microbiomes containing Lachnospiraceae were linked to an increase in fecal carbohydrates. Thus, a gut microbiota dominated by Lachnospiraceae was linked to insulin resistance as well as feces high in monosaccharides. At the same time, people with more Bacteroidales-type bacteria in their stomachs had lower insulin resistance and monosaccharide levels than others.
The team then set out to see the direct effect of bacteria on metabolism in culture and then in mice. In culture, Bacteroidales bacteria consumed the same kinds of monosaccharides that were found in the feces of people with high insulin resistance, with the species Alistipes indistinctus consuming the greatest variety. In obese mice, the team looked at how treatment with different bacteria affected blood sugar levels. They found that A. indistinctus lowered blood sugar and reduced insulin resistance and the amount of carbohydrates available to the mice.
These findings agreed with those of human patients and have implications for diagnosis and treatment. “Because of its association with insulin resistance, the presence of gut Lachnospiraceae bacteria could be a good biomarker for pre-diabetes,” adds Ohno. Similarly, probiotics containing A. indistinctus may alleviate glucose intolerance in people with pre-diabetes.”
Although the bacteria identified in this study are not currently found in most over-the-counter probiotics, Ohno advises caution if they become available. “These findings must be confirmed in human clinical trials before we can recommend any probiotic as an insulin resistance treatment.”