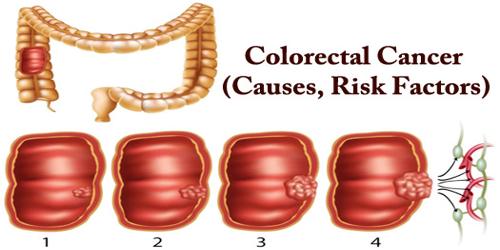
Colorectal cancer (CRC), also known as bowel cancer, colon cancer, or rectal cancer, is a type of cancer that begins in the large intestine (colon). The colon is the final part of the digestive tract. Cancer is the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Signs and symptoms may include blood in the stool, a change in bowel movements, weight loss, and feeling tired all the time.
The American Cancer Society estimates that about 1 in 21 men and 1 in 23 women in the United States will develop colorectal cancer during their lifetime. It is the second leading cause of cancer death in women, and the third for men. However, due to advances in screening techniques and improvements in treatments, the death rate from colorectal cancer has been falling.
Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancers. Other risk factors include diet, obesity, smoking, and lack of physical activity. Dietary factors that increase the risk include red meat, processed meat, and alcohol. Another risk factor is inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis. Some of the inherited genetic disorders that can cause colorectal cancer include familial adenomatous polyposis and hereditary non-polyposis colon cancer; however, these represent less than 5% of cases. It typically starts as a benign tumor, often in the form of a polyp, which over time becomes cancerous.
Colorectal cancer may be benign, or non-cancerous, or malignant. Malignant cancer can spread to other parts of the body and damage them. Many treatments are available to help control it, including surgery, radiation therapy and drug treatments, such as chemotherapy, targeted therapy, and immunotherapy.
Causes –
Doctors aren’t certain what causes most colon cancers. In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell’s DNA contains a set of instructions that tell a cell what to do. Greater than 75–95% of colorectal cancer occurs in people with little or no genetic risk.
People with inflammatory bowel disease (ulcerative colitis and Crohn’s disease) are at increased risk of colon cancer. People with inflammatory bowel disease account for less than 2% of colon cancer cases yearly. In those with Crohn’s disease, 2% get colorectal cancer after 10 years, 8% after 20 years, and 18% after 30 years. In people who have ulcerative colitis, approximately 16% develop either a cancer precursor or cancer of the colon over 30 years.
Healthy cells grow and divide in an orderly way to keep our bodies functioning normally. But when a cell’s DNA is damaged and becomes cancerous, cells continue to divide even when new cells aren’t needed. As the cells accumulate, they form a tumor.
With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Risk factors –
Factors that may increase our risk of colon cancer include:
- older age
- a diet that is high in animal protein, saturated fats, and calories
- a diet that is low in fiber
- high alcohol consumption
- having had breast, ovary, or uterine cancer
- a family history of colorectal cancer
- having ulcerative colitis, Crohn’s disease, or irritable bowel disease (IBD)
- overweight and obesity
- smoking
- a lack of physical activity
- the presence of polyps in the colon or rectum, as these may eventually become cancerous.
Most colon cancers develop within polyps (adenoma). These are often found inside the bowel wall. Eating red or processed meats may increase the risk. People who have a tumor suppressor gene known as Sprouty2 may have a higher risk of colorectal cancers.
According to WHO (World Health Organization), colorectal cancer is the second most common tumor among both men and women, after lung tumors. Around 2 percent of people aged over 50 years will eventually develop colorectal cancer in Western Europe.
Colorectal cancer tends to affect men and women equally. However, men tend to develop it at a younger age.
Epidemiology –
Globally more than 1 million people get colorectal cancer every year resulting in about 715,000 deaths as of 2010 up from 490,000 in 1990.
As of 2012, it is the second most common cause of cancer in women (9.2% of diagnoses) and the third most common in men (10.0%) with it being the fourth most common cause of cancer death after lung, stomach, and liver cancer. It is more common in developed than in developing countries. Globally incidences vary 10-fold with the highest rates in Australia, New Zealand, Europe, and the US and lowest rates in Africa and South-Central Asia.
Information Sources: