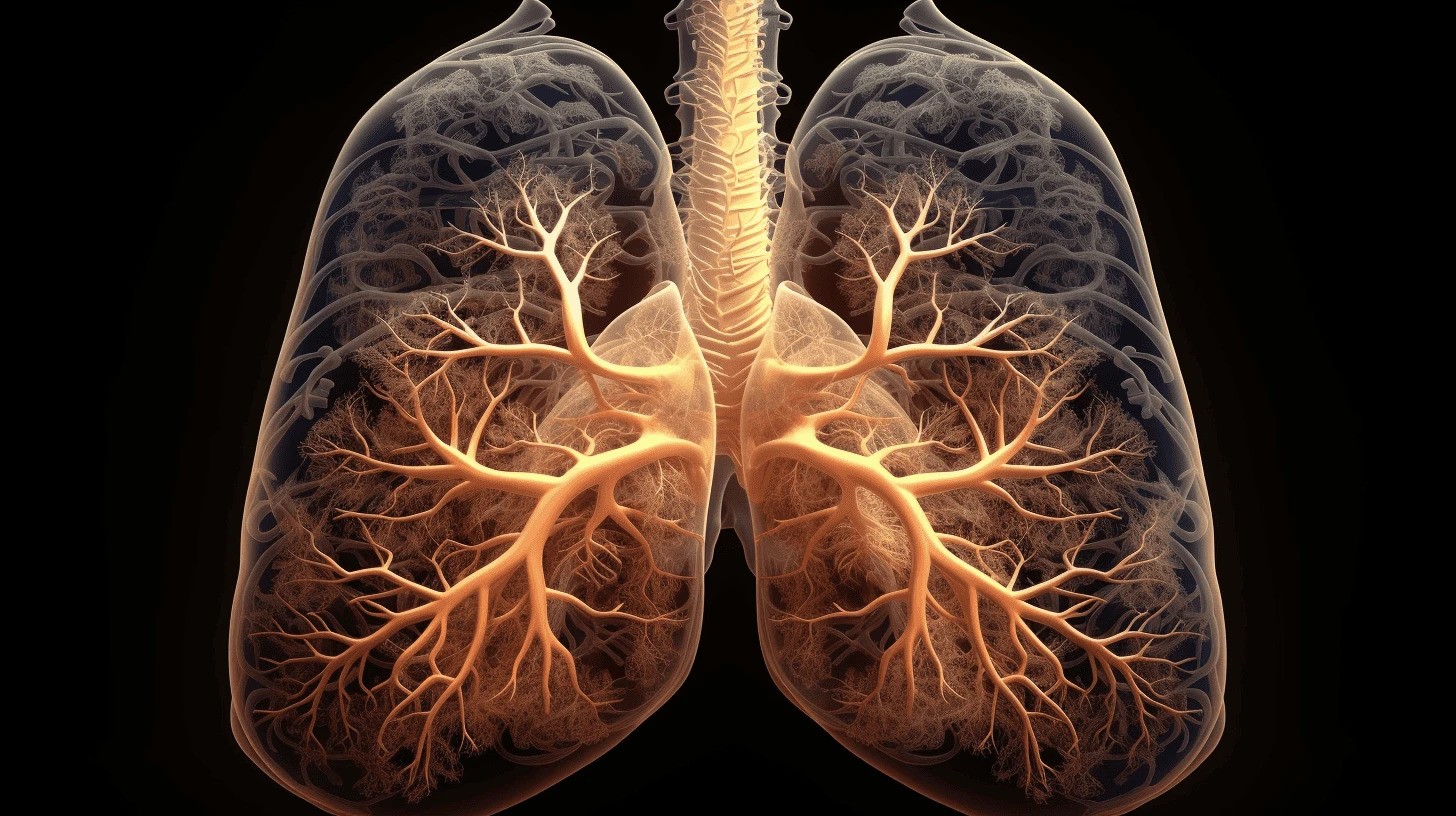
A saliva test can more accurately predict the severity of recurring respiratory infections in children than a normal blood test. A youngster is more likely to get pneumonia if his or her saliva includes a low level of broadly protective antibodies. Researchers from Radboudumc Amalia Children’s Hospital and UMC Utrecht Wilhelmina Children’s Hospital published their findings in the European Respiratory Journal. Saliva testing gives vital therapeutic information while also being more comfortable for youngsters.
About ten to fifteen percent of all youngsters have recurring respiratory infections. When patients go to the hospital, blood is obtained to check for antibody deficits as an underlying problem. However, this rarely produces useful results. “This is challenging for pediatricians because we really want to help the children,” says Lilly Verhagen, a pediatric infectious disease specialist/immunologist at Radboud University Medical Center. As a result, we looked into different options for learning more about the disease’s severity. That would be really helpful in assessing which children require further attention and when antibiotics should be administered.’
A study of one hundred children with recurrent respiratory infections found that saliva measurements predict disease severity better than blood measurements. ‘There was no link between blood antibodies and disease burden. However, we discovered widely protective antibodies in saliva that function against a number of infections.
Lilly Verhagen
Broad Protection
A study of one hundred children with recurrent respiratory infections found that saliva measurements predict disease severity better than blood measurements. ‘There was no link between blood antibodies and disease burden. However, we discovered widely protective antibodies in saliva that function against a number of infections. Children who had lower levels of these antibodies experienced more severe illnesses. “These antibodies in saliva are a good indicator of disease burden,” says PhD student Mischa Koenen.
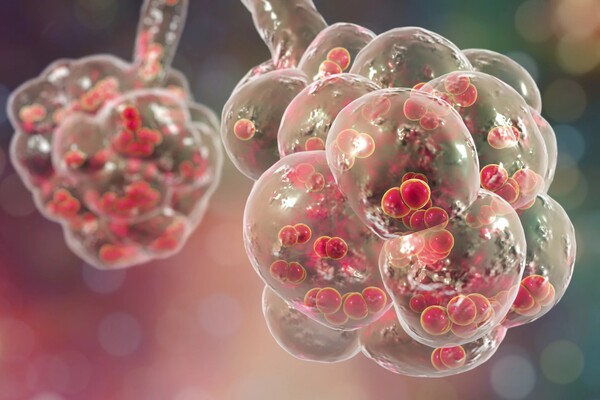
The broadly protective antibodies are present in everyone’s airways; researchers also found them in siblings and parents of the affected children and in healthy caregivers. A high level of these antibodies in saliva is beneficial against respiratory infections. Theybind so broadly that researchers found antibodies in pre-pandemic children’s saliva that could bind to the SARS-CoV-2 virus.
Bacteria
While highly present in saliva, the broadly protective antibodies are scarcely identified in the blood. ‘And that’s quite logical’, says Verhagen. ‘You inhale various things all day, including many respiratory pathogens, and therefore need a broad spectrum of antibodies in your airways. It’s different in the blood: only few pathogens enter the bloodstream through the mucosa of the intestines or airways. When that happens, your body benefits more from a strong, targeted immune response.’
Aside from antibodies, the researchers investigated the balance of beneficial and potentially harmful microorganisms on the mucous membranes of the airways, generally known as the microbiome. They discovered that a specific bacterium on the nasopharyngeal mucosa had a substantial correlation with the severity of respiratory illnesses. This bacterium, Haemophilus influenzae, can also colonize healthy airways. However, children with a high abundance of this bacterium on their airway mucosa are more likely to become unwell during the winter. This bacterium has previously been connected to pneumonia cases.
Future
Saliva and nasopharyngeal mucosal measures are thus extremely useful in diagnosing children with recurring respiratory infections. According to Koenen, “This allows us to determine how much care and medication children require, as well as which antibiotic to use, because the current standard does not work optimally against Haemophilus influenzae.” I expect the initial blood test to continue, but for follow-up appointments, a more child-friendly saliva and nasopharyngeal swab might be utilized to predict respiratory illness burden.
Saliva testing also opens up possibilities for new treatments and therapies. The researchers discovered that the flu vaccine boosts the number of broadly protective antibodies in the saliva of healthy caretakers. In addition, the researchers are investigating the long-term viability of using these antibodies to treat respiratory infections.