An uncovered protein’s pathway, according to researchers at Queen’s University Belfast, may enable early detection and focused therapy for a number of malignancies and brain illnesses.
The research team found that an identified protein’s journey or molecular pathway is crucial for brain development and that changing this pathway could lead to the spread of cancer.
The research, which was just published in Nature Cell Biology, uncovered the molecular pathways underlying a coordinated and timed movement of cells that is crucial for the migration of developing neurons in the brain and can also spread cancer or induce cancer metastases across the body.
The discovery is anticipated to have a significant impact on the fundamental knowledge of cancer metastasis and brain development and could result in an earlier diagnosis and improved treatments, according to the study’s authors.
Neural stem cells produce neurons throughout brain development, which subsequently move to particular regions of the brain where they connect and develop in function. Numerous neurodevelopment problems are known to be brought on by a flaw in this process. Decoding the basic mechanics of brain development and unveiling new diagnostic and treatment options for these illnesses depend on a better comprehension of these occurrences.
Roughly 10 million deaths, or nearly one in six deaths, will be caused by cancer in 2020, making it the top cause of death globally. The majority of tumours are solid, except for a few cancer types of blood origin.
When solid tumors are discovered, it’s common for some of the primary tumor’s cells to have already started to metastasize, or spread to other parts of the body, resulting in secondary tumors, the cells of which are frequently chemotherapy-resistant.
While the primary tumor can be targeted with surgical excision, chemotherapy, and other anti-tumor therapies, metastasis makes the prognosis unclear and can cause a more dramatic relapse. It is crucial to understand the features of cancer in order to tackle it.
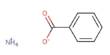
The molecular route known as epithelial to mesenchymal transition (EMT) promotes cell migration and is crucial for early developmental processes, such as brain formation, as well as for the healing of wounds later in life. Cancer cells also use EMT for metastasis.
Our study not only sheds light on the development of one of the most important organs in our body the brain but it also shows how the same protein that is key for brain development can also be the cause or target for the spread of cancer in the body, a real Jekyll and Hyde protein.
Dr. Vijay Tiwari
The research group identified ZNF827 as a specific protein that is an important regulator of EMT. The study demonstrates how the protein’s journey or molecular pathway is used by both tumor cells to gain the ability to migrate and consequently induce metastasis to various organs, as well as by newborn neurons to migrate to the appropriate locations during brain development.
Lead Author, Dr. Vijay Tiwari from the Wellcome-Wolfson Institute for Experimental Medicine at Queen’s University, said: “Our study not only sheds light on the development of one of the most important organs in our body the brain but it also shows how the same protein that is key for brain development can also be the cause or target for the spread of cancer in the body, a real Jekyll and Hyde protein.”
“The process for migrating newborn neurons to proper places during brain development is the same process exploited by tumour cells to gain migration potential, causing the movement of cancer throughout the body, or cancer metastasis.”
“By identifying key regulators of these pathways, we open new opportunities for a therapeutic intervention against cancer and a better understanding of neurodevelopmental disorders involving defects in brain development.”
The international team includes researchers from Queen’s University Belfast, Salk Institute for Biological Studies, Altos Labs, University of Montpellier, Karolinska Institutet, University Medical Center of the Johannes Gutenberg University Mainz and Translational Oncology at the University Medical Center of the Johannes Gutenberg University Mainz gGmbH (TRON gGmbH).
The Deutsche Forschungsgemeinschaft, Wilhelm Sander Stiftung and Innovation supported this study to Commercialisation of University Research program.