INTRODUCTION
Background:
Breastfeeding is an unequaled way of providing ideal food for the healthy growth and development of infants; it is also an integral part of the reproductive process with important implications for the health of mothers. Review of evidence has shown that, on a population basis, exclusive breastfeeding for 6 months is the optimal way of feeding infants. Thereafter infants should receive complementary foods with continued breastfeeding up to 2 years of age or beyond.
Breast milk is the natural first food for babies, it provides all the energy and nutrients that the infant needs for the first months of life, and it continues to provide up to half or more of a child’s nutritional needs during the second half of the first year, and up to one-third during the second year of life.
Exclusive breastfeeding in the first six months, continued till 11 months would prevent 13 percent of all deaths of children below five years of age in low-income countries (The daily star, 24.06.2011). Breast milk promotes sensory and cognitive development, and protects the infant against infectious and chronic diseases. Exclusive breastfeeding reduces infant mortality due to common childhood illnesses such as diarrhoea or pneumonia, and helps for a quicker recovery during illness.
Breastfeeding contributes to the health and well-being of mothers; it helps to space children, reduces the risk of ovarian cancer and breast cancer, increases family and national resources, is a secure way of feeding and is safe for the environment.
Though Bangladesh has a culture of breast-feeding, there are problems regarding lack of awareness over the right time to start nursing and complementing it with other digestible food. World Health Organisation (WHO) recommends exclusive breastfeeding in the first six months of a baby’s birth. Forty-three percent of infants under six months of age in the country are exclusively breastfed only for two months. Infant and Young Child Feeding (IYCF) (a UNICEF global strategy on child nutrition), also, highly recommends that infants should not be given any sort of liquid or semi-liquid food other than breast milk until six months. But more than half of breastfed children under six months receive water, juices, other milks or complementary food and 20 percent are receiving solid or semi-solid foods. IYCF practices suggest introducing complementary food for a child beside breast milk only when a child is six months old. This reduces the risk of malnutrition. Most of the mothers in Bangladesh breastfeed their infants, but they rarely practice exclusive breastfeeding.
Objective of the study
General objective of the study is to assess the level of knowledge and extent of practice about exclusive breast feeding among the mothers attending in Dhaka Shishu Hospital in Dhaka. Specific objectives of the study are given below:
- To determine the socio demographic characteristics of the mother
- To assess the level of knowledge of the mothers about exclusive breast feeding
- To assess the level of knowledge of the mothers about colostrums
- To estimate the extent of practice of exclusive breast feeding among the respondent mothers
- Give recommendation to increase awareness among the mothers about exclusive breast feeding.
Justification of the study
Breastfeeding is fundamental to the health and development of children and important for the health of their mothers. Infants who are exclusively breastfed are less likely to be exposed to contaminated foods and liquids, and this contributes to reductions in the incidence and severity of infectious diseases. The programme for control of diarrhea diseases has long recognized the need the promotion of exclusive breast feeding in the first to 6 months of life, and sustained breast feeding to together with adequate complementary foods up to 2 years of age or beyond, reduce diarrhea morbidly and mortality.
Currently, the recommendation from the Global Strategy for Infant and Young Child Feeding, developed by World Health Organization (WHO) and United Nations Children’s Fund (UNICEF), is that infants should be exclusively breastfed for the first six months of life. After six months, infants should receive nutritionally adequate and safe complementary foods while continuing to be breastfed for up two years of age or beyond.
Recent estimates predict that current breastfeeding patterns are far below the recommended levels especially in Africa and Asia where rates of exclusive breastfeeding for the first six months are less than 40%. In Bangladesh, infections diseases, such as diarrhea and acute respiratory infections are a cause of more than two thirds of all deaths in children aged less than one year.
Bangladesh is considered as a developing economy which has recorded GDP growth above 5% during the last few years. Microcredit has been a major driver of economic development in Bangladesh and although three fifths of Bangladeshis are employed in the agriculture sector, three quarters of exports revenues come from garment industry. The biggest obstacles to sustainable development in Bangladesh are overpopulation, poor infrastructure, corruption, political instability and a slow implementation of economic reforms. According to World Bank, exclusive breast feeding rate in Bangladesh in the year 2009 is 42.9% which is far below than that of the developed countries. The situation is even worse in the northern part of Bangladesh where it is well known for its poor nutritional status. In compared to the other part of Bangladesh, the level of IQ is lower in the northern Bangladesh. Lack of practice of exclusive breast feeding is considered one of the major contributors to this problem.
To help develop a future generation with proper cognitive development it is necessary to increase awareness among the mothers about the necessity of exclusive breast feeding which will increase the extent of practice. The purpose of the study is to determine and explore the level of knowledge of the mothers about exclusive breast feeding. The findings of the study will help the policy maker to develop a proper need based awareness raise campaign among the mother about exclusive breast feeding which ultimately will reduce the chance of occurrence of diarrhea and infectious diseases and protect malnutrition and help develop a better future generation. This will consequently make the northern Bangladesh and hence, country a prosperous one.
Limitation of the study
The limitations of the study are listed below:
- Due to time constraint this research could not take a good sample size.
- Prior relevant studies for the study area were not available.
- Relevant data was not available.
- As most of the respondent mothers were from rural household so it was very difficult to collect information through questionnaire survey. The respondents were very reserved and felt shy telling about breast feeding.
LITERATURE REVIEW
Exclusive breastfeeding:
Breastfeeding is the feeding of an infant or young child with breast milk directly from female human breasts (i.e., via lactation) rather than from a baby bottle or other container. Babies have a sucking reflex that enables them to suck and swallow milk. It is recommended that mothers breastfeed for six months or more, without the addition of infant formula or solid food. This is known as exclusive breastfeeding. After the addition of solid food, mothers are advised to continue breast-feeding up to a year, and can continue for two years or more.
Human breast milk is the healthiest form of milk for babies (Picciano, 2001). There are few exceptions, such as when the mother is taking certain drugs or is infected with human T-lymphotropic virus, HIV, or has active untreated tuberculosis. Breastfeeding promotes health and helps to prevent disease (Falco, 2010). Artificial feeding is associated with more deaths from diarrhea in infants in both developing and developed countries (Horton, 1996). Experts agree that breastfeeding is beneficial, and have concerns about artificial formulas but there are conflicting views about how long exclusive breastfeeding remains beneficial (Krammer, 2002).
The World Health Organization (WHO) and the American Academy of Pediatrics (AAP) emphasize the value of breastfeeding for mothers as well as children. Both recommend exclusive breastfeeding for the first six months of life and then supplemented breastfeeding for at least one year and up to two years or more (WHO, 2003).
Not all the properties of breast milk are understood, but its nutrient content is relatively stable. Breast milk is made from nutrients in the mother’s bloodstream and bodily stores. Breast milk has just the right amount of fat, sugar, water, and protein that is needed for a baby’s growth and development. Because breastfeeding uses an average of 500 calories a day it helps the mother lose weight after giving birth (Dewey, 1993). The composition of breast milk changes depending on how long the baby nurses at each session, as well as on the age of the child.
Benefits of exclusive breastfeeding for the infants
Scientific research, such as the studies summarized in a 2007 review for the U.S. Agency for Healthcare Research and Quality (AHRQ) (Chung, 2007) and a 2007 review for the WHO (Horta, 2007), has found many benefits to breastfeeding for the infant. These include:
Greater immune health
During breastfeeding, antibodies pass to the baby. This is one of the most important features of colostrum, the breast milk created for newborns. Breast milk contains several anti-infective factors such as bile salt stimulated lipase (protecting against amoebic infections), lactoferrin (which binds to iron and inhibits the growth of intestinal bacteria [Kunz, 1999]) and immunoglobulin A protecting against microorganisms (Glass, 1983).
Fewer infections
Among the studies showing that breastfed infants have a lower risk of infection than non-breastfed infants are:
- In a 1993 University of Texas Medical Branch study, a longer period of breastfeeding was associated with a shorter duration of some middle ear infections (otitis media with effusion) in the first two years of life (Owen, 1993).
- A 1995 study of 87 infants found that breastfed babies had half the incidence of diarrheal illness, 19% fewer cases of any otitis media infection, and 80% fewer prolonged cases of otitis media than formula fed babies in the first twelve months of life (Dewey, 1995).
- Breastfeeding appeared to reduce symptoms of upper respiratory tract infections in premature infants up to seven months after release from hospital in a 2002 study of 39 infants (Blaymore, 2002).
- A 2004 case-control study found that breastfeeding reduced the risk of acquiring urinary tract infections in infants up to seven months of age, with the protection strongest immediately after birth (Marild, 2004).
- The 2007 review for AHRQ found that breastfeeding reduced the risk of acute otitis media, non-specific gastroenteritis, and severe lower respiratory tract infections (Chung, 2007).
Protection from SIDS
Breastfed babies have better arousal from sleep at 2–3 months. This coincides with the peak incidence of sudden infant death syndrome (Horne, 2004). A study conducted at the University of Münster found that breastfeeding halved the risk of sudden infant death syndrome in children up to the age of 1 (Vennemann, 2007).
Higher intelligence
Studies have examined whether breastfeeding in infants is associated with higher intelligence later in life. Many have found a connection:
- Horwood, Darlow and Mogridge (2001) tested the intelligence quotient (IQ) scores of 280 low birthweight children at seven or eight years of age. Those who were breastfed for more than eight months had verbal IQ scores 6 points higher (which was significantly higher) than comparable children breastfed for less time. They concluded “These findings add to a growing body of evidence to suggest that breast milk feeding may have small long term benefits for child cognitive development” (Horwood, 2001).
- A 2005 study using data on 2,734 sibling pairs from the National Longitudinal Study of Adolescent Health “provide[d] persuasive evidence of a causal connection between breastfeeding and intelligence.” The same data “also suggests that non-experimental studies of breastfeeding overstate some of [breastfeeding’s] other long-term benefits, even if controls are included for race, ethnicity, income, and education” (Evenhouse, 2005).
- The 2007 review for the WHO “suggests that breastfeeding is associated with increased cognitive development in childhood.” The review also states that “The issue remains of whether the association is related to the properties of breastmilk itself, or whether breastfeeding enhances the bonding between mother and child, and thus contributes to intellectual development” (Horta, 2007).
- Two initial cohort studies published in 2007 suggest babies with a specific version of the FADS2 gene demonstrated an IQ averaging 7 points higher if breastfed, compared with babies with a less common version of the gene who showed no improvement when breastfed. FADS2 affects the metabolism of polyunsaturated fatty acids found in human breast milk, such as docosahexaenoic acid and arachidonic acid, which are known to be linked to early brain development. The researchers were quoted as saying “Our findings support the idea that the nutritional content of breast milk accounts for the differences seen in human IQ. But it’s not a simple all-or-none connection: it depends to some extent on the genetic makeup of each infant.” The researchers wrote “further investigation to replicate and explain this specific gene–environment interaction is warranted” (Capsi, 2007).
- In “the largest randomized trial ever conducted in the area of human lactation,” between 1996 and 1997 maternity hospitals and polyclinics in Belarus were randomized to receive or not receive breastfeeding promotion modeled on the Baby Friendly Hospital Initiative. Of 13,889 infants born at these hospitals and polyclinics and followed up in 2002-2005, those who had been born in hospitals and polyclinics receiving breastfeeding promotion had IQs that were 2.9-7.5 points higher (which was significantly higher). Since (among other reasons) a randomized trial should control for maternal IQ, the authors concluded in a 2008 paper that the data “provide strong evidence that prolonged and exclusive breastfeeding improves children’s cognitive development.” (Krammer, 2007).
Less diabetes
Infants exclusively breastfed have less chance of developing diabetes mellitus type 1 than peers with a shorter duration of breastfeeding and an earlier exposure to cow milk and solid foods (Perez Bravo, 1996). Breastfeeding also appears to protect against diabetes mellitus type 2, at least in part due to its effects on the child’s weight (M Davis, 2008).
Less childhood obesity
Breastfeeding appears to reduce the risk of extreme obesity in children aged 39 to 42 months (Armstrong, 2002). The protective effect of breastfeeding against obesity is consistent, though small, across many studies, and appears to increase with the duration of breastfeeding (Arenz, 2004). A study has also shown that infants who are bottle-fed in early infancy are more likely to empty the bottle or cup in late infancy than those who are breastfed. “Bottle-feeding, regardless of the type of milk, is distinct from feeding at the breast in its effect on infants’ self-regulation of milk intake.” According to the study, this may be due to one of three possible factors, including that when bottle feeding, parents may encourage an infant to finish the contents of the bottle whereas when breastfeeding, an infant naturally develops self-regulation of milk intake (Li R, 2010).
Less tendency to develop allergic diseases (atopy)
In children who are at risk for developing allergic diseases (defined as at least one parent or sibling having atopy), atopic syndrome can be prevented or delayed through exclusive breastfeeding for four months, though these benefits may not be present after four months of age (Greer, 2008). However, the key factor may be the age at which non-breastmilk is introduced rather than duration of breastfeeding (Oddy, 1999). Atopic dermatitis, the most common form of eczema, can be reduced through exclusive breastfeeding beyond 12 weeks in individuals with a family history of atopy, but when breastfeeding beyond 12 weeks is combined with other foods incidents of eczema rise irrespective of family history (Pratt, 1984)
Benefits for mothers
Breastfeeding is a cost effective way of feeding an infant, providing nourishment for a child at a small cost to the mother. Frequent and exclusive breastfeeding can delay the return of fertility through lactational amenorrhea, though breastfeeding is an imperfect means of birth control. During breastfeeding beneficial hormones are released into the mother’s body and the maternal bond can be strengthened. Breastfeeding is possible throughout pregnancy, but generally milk production will be reduced at some point. (Feldman, 2000)
Bonding
Hormones released during breastfeeding help to strengthen the maternal bond. Teaching partners how to manage common difficulties is associated with higher breastfeeding rates (Pisacane, 2005). Support for a mother while breastfeeding can assist in familial bonds and help build a paternal bond between father and child (W Van, 2002).
If the mother is away, an alternative caregiver may be able to feed the baby with expressed breast milk. The various breast pumps available for sale and rent help working mothers to feed their babies breast milk for as long as they want. To be successful, the mother must produce and store enough milk to feed the child for the time she is away, and the feeding caregiver must be comfortable in handling breast milk.
Hormone release
Breastfeeding releases oxytocin and prolactin, hormones that relax the mother and make her feel more nurturing toward her baby (Stuart, 1995). Breastfeeding soon after giving birth increases the mother’s oxytocin levels, making her uterus contract more quickly and reducing bleeding. Pitocin, a synthetic hormone used to make the uterus contract during and after labour, is structurally modelled on oxytocin. Syntocinon, another synthetic oxytocic, is commonly used in Australia and the UK rather than Pitocin (Chua S, 1994).
Weight loss
As the fat accumulated during pregnancy is used to produce milk, extended breastfeeding—at least 6 months—can help mothers lose weight (Dewey, 1993). However, weight loss is highly variable among lactating women; monitoring the diet and increasing the amount/intensity of exercise are more reliable ways of losing weight (Lovelady, 2000). The 2007 review for the AHRQ found “The effect of breastfeeding in mothers on return-to-pre-pregnancy weight was negligible, and the effect of breastfeeding on postpartum weight loss was unclear” (Ip S, 2007).
Natural postpartum infertility
Breastfeeding may delay the return to fertility for some women by suppressing ovulation. A breastfeeding woman may not ovulate, or have regular periods, during the entire lactation period. The period in which ovulation is absent differs for each woman. This lactational amenorrhea has been used as an imperfect form of natural contraception, with greater than 98% effectiveness during the first six months after birth if specific nursing behaviors are followed (Price, 2004). It is possible for women to ovulate within two months after birth while fully breastfeeding and get pregnant again.
Long-term health effects
For breastfeeding women, long-term health benefits include:
- Less risk of breast cancer, ovarian cancer, and endometrial cancer (Newcomb 2000).
- A 2009 study indicated that lactation for at least 24 months is associated with a 23% lower risk of coronary heart disease (Stuebe, 2009).
- Although the 2007 review for the AHRQ found “no relationship between a history of lactation and the risk of osteoporosis”, mothers who breastfeed longer than eight months benefit from bone re-mineralisation (Melton, 1993).
- Breastfeeding diabetic mothers require less insulin (Rayburn, 1985).
- Reduced risk of metabolic syndrome (Gunderson, 2009).
- Reduced risk of post-partum bleeding (Chua S, 1994).
- According to a Malmö University study published in 2009, women who breast fed for a longer duration have a lower risk for contracting rheumatoid arthritis than women who breast fed for a shorter duration or who had never breast fed (Pikwer, 2009).
Colostrums
Colostrum (also known colloquially as beestings, bisnings or first milk) is a form of milk produced by the mammary glands of mammals in late pregnancy. Most species will generate colostrum just prior to giving birth. Human and bovine colostrums are thick, sticky and yellowish. Colostrum contains antibodies to protect the newborn against disease, as well as being lower in fat and higher in protein than ordinary milk (L. Saint, 1984).
In humans, it has high concentrations of nutrients and antibodies, but it is small in quantity. Colostrum is high in carbohydrates, high in protein, high in antibodies, and low in fat (as human newborns may find fat difficult to digest).
Benefits of Colostrums
Newborns have very small digestive systems, and colostrum delivers its nutrients in a very concentrated low-volume form.
It has a mild laxative effect, encouraging the passing of the baby’s first stool, which is called meconium. This clears excess bilirubin, a waste product of dead red blood cells, which is produced in large quantities at birth due to blood volume reduction, from the infant’s body and helps prevent jaundice.
Colostrum is known to contain antibodies called immunoglobulins such as IgA, IgG, and IgM in mammals. IgA is absorbed through the intestinal epithelium, travels through the blood, and is secreted onto other Type 1 mucosal surfaces. These are the major components of the adaptive immune system.
Other immune components of colostrum include the major components of the innate immune system, such as lactoferrin, lysozyme, lactoperoxidase, complement, and proline-rich polypeptides (PRP). A number of cytokines (small messenger peptides that control the functioning of the immune system) are found in colostrum as well, including interleukins, tumor necrosis factor, chemokines, and others.
Leukocytes are also present in large numbers in colostrums; these begin protecting the infant from harmful viruses and bacteria.
Ingesting colostrum establishes beneficial bacteria in the digestive tract. Premature babies tend to fare better on human colostrum than commercial infant formulas.
Colostrum also contains a number of growth factors, such as insulin-like growth factors I, and II, transforming growth factors alpha, beta 1 and beta 2, fibroblast growth factors, epidermal growth factor, granulocyte-macrophage-stimulating growth factor, platelet-derived growth factor, vascular endothelial growth factor, and colony-stimulating factor-1 (Fidel-Rimon, 1997).
Colostrum is very rich in proteins, vitamin A, and sodium chloride, but contains lower amounts of carbohydrates, lipids, and potassium than normal milk. The most pertinent bioactive components in colostrum are growth factors and antimicrobial factors. The antibodies in colostrum provide passive immunity, while growth factors stimulate the development of the gut. They are passed to the neonate and provide the first protection against pathogens.
Human milk contains special components, called growth modulators, that help the premature baby’s digestive system adjust to oral feedings.
Related Study
Leia M. Chatman et al conducted a cross sectional study in 11 health centers within the parish of Saint Ann, Jamaica to gather information about factors that influence exclusive breastfeeding and its duration. Information was collected and documented for 599 mother-child pairs through questionnaire survey. From the study it has been found that the prevalence of breastfeeding initiation was 98.2 percent; of mothers who initiated breastfeeding, 22.2 percent practiced it exclusively (at least 6 months). No difference occurred between exclusive and nonexclusive breastfeeding mothers in terms of knowledge about and attitudes toward breastfeeding. Of potential predictors assessed, the male partner’s role as the main source of income for the family was the only significant predictor for exclusive breastfeeding. Women whose male partner was the main source of income for the family were twice as likely to exclusively breastfeed their infants compared with the referent group (mothers as main source of income) (OR = 2.0; 95% CI = 1.4–3.0). In addition, the dominant reason for partial breastfeeding was maternal anxiety that breastmilk alone might not provide sufficient nourishment. The level of exclusive breastfeeding was extremely low at the study site. Formulation of strategies to aggressively promote exclusive breastfeeding practices is urgently needed there. Such interventions should consider involvement of the male partner, especially, with respect to the financial support, as well as alleviating maternal anxiety regarding nutritional adequacy of breastmilk. (Leia M, et al, 2004)
To describe breastfeeding practices and investigate the influence of exclusive breastfeeding in early infancy on the risk of infant deaths, especially those attributable to respiratory infections (ARI) and diarrhea Shams Arifeen and et al conducted a prospective observational study on a birth cohort of 1677 infants who were born in slum areas of Dhaka in Bangladesh and followed from birth to 12 months of age. After enrollment at birth, the infants were visited 5 more times by 12 months of age. Verbal autopsy, based on a structured questionnaire, was used to assign a cause to the 180 reported deaths. Proportional hazards regression models were used to estimate the effect of breastfeeding practices, introduced as a time-varying variable, after accounting for other variables, including birth weight. Overall neonatal, post neonatal and infant mortality, and mortality attributable to ARI and diarrhea were measured. The proportion of infants who were breastfed exclusively was only 6% at enrollment, increasing to 53% at 1 month and then gradually declining to 5% at 6 months of age. Predominant breastfeeding declined from 66% at enrollment to 4% at 12 months of age. Very few infants were not breastfed, whereas the proportion of partially breastfed infants increased with age. Breastfeeding practices did not differ between low and normal birth weight infants at any age. The overall infant mortality rate was 114 deaths per 1000 live births. Compared with exclusive breastfeeding in the first few months of life, partial or no breastfeeding was associated with a 2.23-fold higher risk of infant deaths resulting from all causes and 2.40- and 3.94-fold higher risk of deaths attributable to ARI and diarrhea, respectively (Shams A, et al, 2001).
METHODOLOGY
Type of the study
This is basically a primary study where data and information were collected through interview and questionnaire survey. Secondary study or literature review was conducted to support the findings of the primary study.
Study area
The study area is such selected that it should represents the northern Bangladesh. To represent both urban and rural context, Dhaka shishu hospital in Dhaka has been selected as the study area where patients from both urban and rural areas come to take treatment. Dhaka is situated in the northern Bangladesh and it represents northern part of Bangladesh both demographically and socio-economically. Samples were collected from labor word, children word, outdoor and EPI centre of Dhaka Shishu Hospital.
Duration of the study
The study was conducted from June to December 2012. Although a work schedule was prepared for the convenience of the study but it could not be maintained properly which results in heavy workload at the end of the study period.
Sample size
Total one hundred and eight (108) respondent mothers were interviewed using a structured questionnaire. The sample size calculation follows the following formula:
Where:
n = Sample size estimate
Z = Z for level of significance alpha (at 0.05 level of significance value of Z is 1.96)
p= 50%
q= 1-p
d= acceptable margin of error (0.10)
Actual sample size was= 1.96 x 1.96x 0.5×0.5/0.1×0.10
= 96.04 @ 100
Sampling technique
The purposive but random sampling technique was followed for this study. Purposive sampling was conducted by confining the study area to labor word, children word and EPI centre in Dhaka Sadar Hospital. From the selected study area the respondents were collected randomly.
Research instrument:
A structured questionnaire was prepared in the light of objectives. The questionnaire was self administered. It was pre-tested. On the basis of experience and expert opinion of my guide the final questionnaire was prepared. The purpose of the study was explained clearly to the respondent before interviewed. One questionnaire was used for each respondent for data collection.
Data Analysis
The data were entered in computer and analyzed with the help of micro-soft excel. According to the study; results have been presented in the forms of chart, table and graph. Descriptive measures such as percentage, frequency were used as summary measures to delineate characteristics of different variables. Based on the findings from the analysis the findings were discussed to come to a conclusion.
RESULTS AND DISCUSSION
RESULTS:
Through questionnaire survey data were collected from randomly selected 108 respondents and analyzed with the help of Microsoft Excel. The results are presented in this chapter.
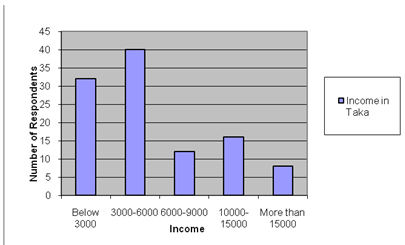
Figure : Income distribution of Respondents
Figure 4.1 shows the income distribution of the respondent’s family. From this figure it has been found that 40% of the respondents’ monthly family income is between 3000 to 6000 taka. Next to this, 32% of the respondents’ income is less than 3000 taka in a month. 12% of the respondents’ family earns 6000-9000 taka per month. Among the total respondents, 16% earns within the range of 10000 to 15000 taka. Only 18% of the respondent’s family income is more than 15000 taka. It reveals that more than 70% of the respondents’ income is less than 6000 taka per month which indicates that they belong to poor family.
Figure 4.2 shows the level of education of the respondents’. From this figure it has been found that most of the respondents, which correspond to 68%, have education of below primary level. Only 15% of the respondents studied beyond primary but could not study until SSC. 20% of the respondents have education level higher than SSC and only 3% passed HSC. As the sampling was random, so it reveals that most of the mother in the district Dinajpur is either illiterate or even if have education but less than primary level.
From the figure 4.3, it has been found that educational qualification of the respondent’s husband is similar to that of the respondents. Majority of the respondent’s husband, 64%, are either illiterate or have education less than class five. Twenty percent (20%) of them acquired SSC level education. Twelve percent and eight percent of the respondent’s husbands have education at the level of HSC and Bachelor respectively.
The figure 4.4 shows the percentage wise involvement in the profession of the respondent’s husband. From this figure it has been found that most of the respondent’s husbands, 40%, are involved with the profession business irrespective of business size. 25% of the respondent’s husbands are engaged in selling day labor. The third biggest group which comprised of 20% of the respondents is involved in agriculture farming. Only 15% of the respondent’s husbands found to be engaged in service and five percent is unemployed although they are responsible for taking care of their own family.
Extent of knowledge of the respondents about exclusive breast feeding
Through the questionnaire survey of 108 respondents, the extent of knowledge of the mothers about exclusive breast feeding has been assessed. From analyzing the answer of a direct question, it has been found that 92% of the respondent mothers have perceived knowledge about exclusive breast feeding which is shown in the figure 4.5.

Figure : percentage of respondents claim that they have perceived knowledge about exclusive breast feeding
Although it has been found from the figure 4.5 that 92% of the respondent mothers have perceived knowledge about exclusive breast feeding but digging deeper into the fact, it reveals that 85% of the mothers know about exclusive breast feeding for children until six months of their age which is shown in the figure 4.7 and from the figure 4.6, it has been found that only 70% of the respondent mothers give breast milk to their children immediately after their birth which is very crucial for infant’s physical and mental health.

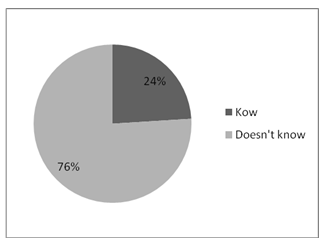
Figure : Perceived knowledge among the mothers about exclusivity of breast milk to the children until six months of their age
Figure 4.8 shows the presence of knowledge among the mothers about the fact that exclusively breast milk should be given to the children until their six months of age. During this period they should not be given any other food. Although figure 4.5, 4.6 and 4.7 show that higher percentage of respondent mothers have idea about exclusive breast feeding but from the figure 4.8, it has been found that only 12% of the respondent mothers know that children should be given only breast milk until six months of their age. The rest 88% of the respondents do not know that breast milk is exclusive until the age of six months.
Extent of knowledge among the respondent mothers about the proper methods and benefits of exclusive breast feeding
Along with the knowledge about exclusive breast feeding, this questionnaire survey also covers the extent of knowledge among the respondent mothers about the benefits of exclusive breast feeding. The result of the analysis with the data collected through questionnaire survey regarding the knowledge about the benefits of exclusive breast feeding, are presented in this section.
Figure 4.9 shows presence of knowledge among the mothers about the proper method of breast feeding to the child. From this figure it has been found that only 24% of the respondent mothers know how to breast feed their children properly while 76% of the respondents do not know the proper method of breast feeding.
Figure 4.10 shows the respondent’s perception about the fact that whether every could breast feed their child. From this figure it has been found that 22% of the respondent mothers know that every mother cannot breast feed their child due to number of reasons while 78% believes that every mother can breast feed their child.
Figure 4.11 shows the respondent’s perception about the fact that whether every mother produces enough milk for their children or not. From this figure it has been found that 83% of the respondent mothers know that every mother does not produces required amount of milk for their child while the rest 17% of the respondents do not know the fact.
Figure 4.12 shows the respondent mothers about perception about the fact that whether pregnant mother could breast feed their child. From this figure, it has been found that 65% of the respondent mothers know that pregnant mother should not breast feed their child while the rest 35% believe that pregnant mother can breast feed their child.
Figure 4.13 shows the perception of the respondent mothers about the fact that feeding milk in bottle is dangerous for infant’s health. From this figure, it has been found that 80% of the respondent mothers are aware about the danger but 20% do not know that it can be harmful.
Figure 4.14 shows the respondents perceived knowledge about the benefit of breast feeding in maintaining family planning. From this figure it has been found that 95% of the respondent mothers do not know that feeding breast milk to their children properly can help maintaining family planning and only 5% of the respondents know the fact.
The figure 4.15 shows the presence of knowledge among the mothers about the ability of breast milk to reduce the chances of attack of diarrhea and pneumonia. From this figure it has been found that only fifteen percent of the respondent mothers know about the capability of breast milk to reduce the chances of attack of diarrhea and pneumonia.
Extent of knowledge among the respondents about the benefits of Colostrums
With the same questionnaire, the extent of knowledge about colostrums and its benefits have been assessed among the respondent mothers. With the questionnaire survey the following results have been found.
Figure 4.16 shows the percentagewise presence of knowledge about colostrums among the respondents. From the figure, it has been found that 70% of the respondent mothers have idea about colostrums and the rest 30% of the respondents have not heard of it before.
With a snapshot view, it has been found that 55% of the respondents have some sort of knowledge about the benefits of colostrums on the children while the rest 45% do not have understanding about the benefits of colostrums although some of the mothers among these 45% have heard about colostrums. This is presented in the figure 4.17 which is shown below.
It is easily conferred from a direct question in the questionnaire that 45% of the respondent mothers have knowledge about the benefits of colostrums. However, to assess their level of knowledge about the benefits of colostrums further questions reveal that only a small portion of the respondents have specific idea about the benefits. Here in this part, respondents’ knowledge has been assessed in specific benefits of the colostrums.
The figure 4.18 shows the respondent mother’s knowledge about the fact that colostrums work as the first anti-biotic for the child. From this figure it has been found that only 20 percent of the respondents know the fact that colostrums can work as the first anti-biotic for the infant. Eighty percent of the mothers do not have any idea about this fact.
Figure 4.19 shows the presence of knowledge among the respondent mothers about the fact that colostrums can increase the children’s immune system. From this figure it has been found that only 23% of the respondent’s know the fact while the other 77% do not have any idea about the fact that colostrums can increase infant’s immune system.
The figure 4.20 shows the presence of knowledge among the respondent mothers about the fact that colostrums can help develop brain of infants. The figure reveals that only 25% of the respondent mothers know about the fact and 75% of the respondents do not have knowledge that colostrums can help develop children’s brain.
Figure 4.21shows the presence of knowledge among the respondent mothers about the fact that colostrums help secreting first black stool (Myconium) of the infants. From this figure it has been found that only eight percent of the respondents know about the fact that colostrums help secreting black stool of the infants while 92% have heard of the fact for the first time.
Figure 4.22 shows the presence of knowledge among the respondent mothers about the fact that colostrums help developing children’s intestine system and increase their digestive power. From the figure it has been found that merely twelve percent of the respondents have knowledge about the fact and 88% of the respondents do not know that colostrums can help developing infant’s intestine system.
Figure 4.23 shows the know how among the respondent mothers about the timing of colostrums secretion. From this figure it has been found that fifty percent of the respondents know the timing of colostrums secretion while the others do not know when colostrums secret.
Extent of Practice of Exclusive Breast Feeding by the Respondent Mothers
Extent of practice of exclusive breast feeding to the infants by the mothers has been assessed with the same hundred and eight samples. Through the questionnaire survey the respondent mother’s practice of breast feeding has been assessed. Whether they provide colostrums to their infant or not has also been assessed through the similar questionnaire survey. The results are shown below:
Figure 4.24 shows the percentage wise practice of respondent mothers in providing breast milk to their child until the age of six months. From this figure it reveals that 75% of the respondent mothers are providing breast milk to their children until the age of six months. This does not mean that this 75% are providing breast milk exclusively. The rest 25% of the respondents are not providing breast milk to their children due to many reasons.
Figure 4.25 shows the practice among the respondent mothers of exclusive breast feeding to their children. From this figure it has been found that only 62% provide exclusively breast milk to their children until their age of six months while the rest 38% are not providing exclusive breast milk to their children which means that among this 38%, some mothers might provide breast milk to their children but not exclusively i.e., besides breast milk they do also provide external formula.
Figure 4.26 shows the percentage of mothers provided colostrums to their infants. From this figure, it reveals that only a small portion of mothers provided colostrums to their infants. It has been found that 46% of the respondent mothers provided colostrums to their infants. The rest 54% of the mothers did not provided colostrums to their infants. Digging deeper into the fact, it disclosed that they were not informed about the benefits of colostrums. Driven by the superstition, colostrums seem something bad which led them to secret out colostrums before giving breast milk to their infants.
DISCUSSION
All the respondents who were interviewed were admitted in Dinajpur Sadar Hospital where patients need not to pay much. As it is a government hospital and the charges for treatment is nominal, so the patients who come for treatment in this hospital are mostly from poor family. From our analysis we also found that more than seventy percent of the respondents were from such a family whose monthly family income were less than six thousand taka and among them fifty percent earn only less than three thousand in a month. Literacy level of the respondents was much lower compared to the average standard. Near about seventy percent of the respondents have less than primary level education. The respondent’s level of education and monthly income definitely have influence on their extent of knowledge about exclusive breast feeding and on their practices. However, this study did not look into the correlationship between the extent of knowledge and respondent’s level of education or their family status. To understand the socio-economic condition of the respondents, their husband’s educational background has also been assessed. More than sixty percent of the respondent’s husbands are either non-educated or have only primary level education.
Although it has been found that 92% of the respondent mothers have perceived knowledge about exclusive breast feeding but digging deeper into the fact, it reveals that 85% of the mothers know about exclusive breast feeding for children until six months of their age. Exploring this fact more deeply has given a frustrating number in reality, about the extent of knowledge regarding exclusive breast feeding. It has been found that only 12% of the respondent mothers know that children should be given only breast milk until six months of their age i.e., only 12% of the respondent mothers have clear understanding regarding exclusive breast feeding. The rest 88% of the respondents do not know that breast milk is exclusive until the age of six months which means that their child should not be given any other food beside breast milk until the age of six months. Knowledge about proper method of breast feeding, what to do and what not to do during breast feeding the child and about the benefits of exclusive breast feeding is also very low.
It has also been found that 70% of the respondent mothers have idea about colostrums and the rest 30% of the respondents have not heard of it before. With a snapshot view, it has been found that 55% of the respondents have some sort of knowledge about the benefits of colostrums on the children while the rest 45% do not have understanding about the benefits of colostrums although some of the mothers among these 45% have heard about colostrums. However, regarding knowledge about specific functioning or specific benefits of colostrums it has been found that respondent’s perception is even poorer. In most cases, on an average only 20% of the respondents knew about the specific functioning of colostrums while in one case this figure is only eight percent.
Regarding practice of exclusive breast feeding, it has been found that 75% of the respondent mothers have provided breast milk to their children until the age of six months but not exclusively while 62% of the total respondents provided exclusively breast milk to their children until their six months of age.
Regarding practice of providing colostrums, it has been found that 46% of the respondent mothers provided colostrums to their infants. The rest 54% of the mothers did not provided colostrums to their infants. Digging deeper into the fact, it disclosed that they were not informed about the benefits of colostrums. Driven by the superstition, colostrums seem something bad which led them to secret out colostrums before giving breast milk to their infants.
In this study, the findings look interesting as the extent of practice of exclusive breast feeding and providing colostrums is much higher than the extent of knowledge regarding these issues. For exclusive breast feeding it can easily be conferred that the practice of exclusive breast feeding is defusing over the generation although most of the mothers are not aware about what they are practicing and why they are practicing this. Regarding provision of colostrums, it is usual that most of the uneducated or slightly educated mother should not know the specific benefits of providing colostrums to the infants. Due to awareness program, some mothers became aware about the necessity of providing colostrums which led them to provide colostrums to their infants.
CONCLUSION AND RECOMMENDATIONS
Conclusion :
This primary study was conducted among one hundred and eight newly been mothers attended in Dinajpur Sadar Hospital for their delivery. After reviewing the findings of the data of this study it is concluded that the majority of the mothers do not have clear understanding about exclusive breast feeding and about colostrums. It is interesting that although their extent of knowledge regarding exclusive breast feeding and colostrums is low but the rate of practice of exclusive breast feeding and providing colostrums is higher.
It has been found that 92% of the respondent mothers have perceived knowledge about exclusive breast feeding but digging deeper into the fact, it reveals that 85% of the mothers know about exclusive breast feeding for children until six months of their age. Exploring this fact more deeply it has been found that only 12% of the respondent mothers know that children should be given only breast milk until six months of their age i.e., only 12% of the respondent mothers have clear understanding regarding exclusive breast feeding. The rest 88% of the respondents do not know that breast milk is exclusive until the age of six months which means that their child should not be given any other food beside breast milk until the age of six months.
It is also found that knowledge about proper method of breast feeding, what to do and what not to do during breast feeding the child and about the benefits of exclusive breast feeding is very low.
The study also explored that 55% of the respondents have some sort of knowledge about the benefits of colostrums on the children while the rest 45% do not have understanding about the benefits of colostrums although some of the mothers among these 45% have heard about colostrums.
The study found that 75% of the respondent mothers have provided breast milk to their children until the age of six months but not exclusively while 62% of the total respondents provided exclusively breast milk to their children until their six months of age.
Regarding practice of providing colostrums, the study has investigated that 46% of the respondent mothers provided colostrums to their infants. The rest 54% of the mothers did not provided colostrums to their infants.
Recommendations:
In the light of findings of the current study, the following recommendations are proposed:
- Mass awareness on the exclusive breast feeding is needed to raise awareness among the newly been mothers.
- There exists a need for awareness campaign on the provision of colostrums.
- Mothers should be informed about the benefits of exclusive breast feeding and colostrums recurrently so that their practice will be improved by believing.
- A detail study is needed to be undertaken to understand the reasons behind and to understand the correlationship between practice and socio-economic condition of the parents.