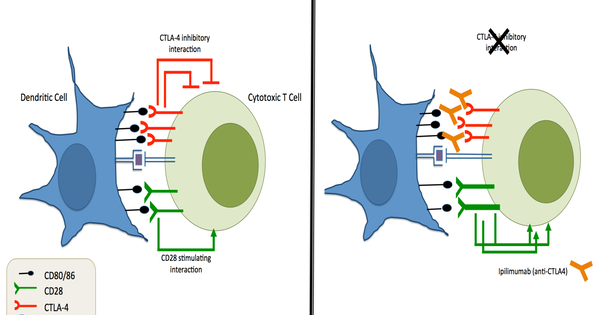
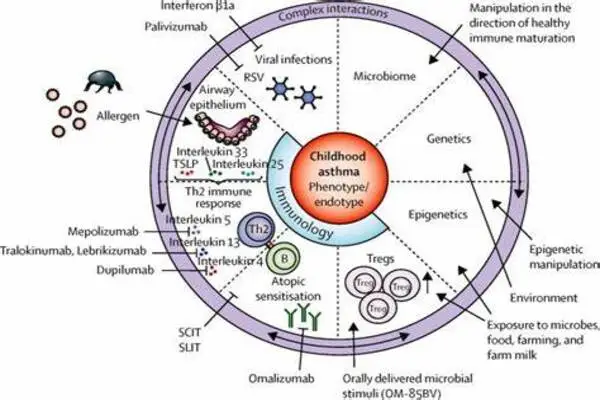
Blocking immune system “messengers” to treat severe asthma is a concept connected to the use of particular biologic drugs in the treatment of severe asthma. These drugs target specific immune system molecules or pathways that play a role in the development of asthma symptoms. Cytokines are a type of molecule that serves as a messenger in the immune system.
Asthma is more hazardous than many people realize. Asthma kills 10 people in the United States every day, and the disease causes 439,000 hospitalizations and 1.3 million emergency room visits each year.
“Asthma is one of the most important allergic diseases to study,” says Professor Toshiaki Kawakami, M.D., Ph.D., a member of the Center for Autoimmunity and Inflammation at La Jolla Institute for Immunology (LJI).
Kawakami and his LJI colleagues explored the molecular causes of severe asthma and rhinovirus-induced asthma exacerbation (a kind of asthma that can accompany a typical cold) in a recent study. Their findings, published recently in The Journal of Allergy and Clinical Immunology, imply that medicines that disrupt interactions between a chemical called histamine-releasing factor (HRF) and antibodies called immunoglobulin E (IgE) may benefit people with both types of asthma.
According to Kawakami, many persons with severe asthma are unresponsive to conventional asthma treatments. He is hopeful that two potential medication methods developed in his research may inhibit HRF and IgE interactions and provide relief to these patients. “We hope to use this approach to treat severe asthma and asthma exacerbations,” he explains.
Asthma is one of the most important allergic diseases to study. We hope to use this approach to treat severe asthma and asthma exacerbations.
Toshiaki Kawakami
The problem with histamine-releasing factor
Immune cells collaborate and produce chemicals to “talk” to one another. HRF is one of these molecular messengers, and it is produced by a variety of cells, including lung epithelial cells and immune cells known as macrophages. When a person is exposed to an allergen, these cells begin producing more HRF. The HRF then travels around the body in search of specific antibodies to bind to. HRF, on the other hand, has a variety of antibody partners, and each contact sends a different message to the surrounding immune cells.
Kawakami and his colleagues are investigating how HRF and antibody interactions cause serious allergic reactions. Over the last decade, researchers have demonstrated that HRF interactions with the IgE antibody cause detrimental inflammation in asthma mice models.
Their new research is significant because it sheds light on how the same HRF and IgE interaction causes inflammation and asthma in humans. Kawakami worked with doctors and scientists from the University Of Pittsburgh School Of Medicine, Children’s Hospital Boston, and the University of Virginia on the study to evaluate the effect of HRF in a variety of patient groups.
The researchers examined HRF levels and IgE interactions in:
- healthy adult controls
- adults infected with rhinovirus
- adults with moderate asthma
- adults with severe asthma
- adults with mild to moderate asthma
- asthmatic children with non-viral asthma exacerbation
- asthmatic children with rhinovirus-induced asthma exacerbation
Working with this large range of patient samples was critical. “Asthma isn’t just one disease,” Kawakami says. There are different forms of asthma, called “endotypes,” and current asthma therapies don’t work for all patients. Truly understanding and treating asthma means gathering data from every patient group possible.
Hope for future therapy
The researchers discovered that HRF and IgE interactions selectively cause inflammation in patients with severe asthma and rhinovirus-induced asthma exacerbation. These findings in humans are consistent with prior findings in animals.
In laboratory trials with a strain of human bronchial cells, the researchers validated the role of HRF and IgE interactions. When Kawakami and his colleagues infected these cells with rhinovirus, they noticed a significant increase in HRF secretion. When scientists exposed the bronchial cells to proteins from house dust mites (a frequent allergen and asthma trigger), they noticed the same substantial rise.
Kawakami currently plans to test two possible asthma treatments. The first strategy would use a chemical created by the Kawakami Lab. This molecule, known as HRF-2CA, appears to reduce asthma and severe food allergy symptoms in mice, and there is reason to believe it could aid in the treatment of humans as well.
The researchers are also interested in researching SPF7-1, a therapeutic antibody that acts as an HRF decoy, attaching to IgE and inhibiting interactions with the genuine HRF.
“The best way forward would be to carry out clinical trials to study these two therapeutic options,” adds Kawakami.