Axial spondyloarthritis
Definition: Axial spondyloarthritis (also often referred to as axSpA) is a type of chronic inflammatory arthritis involving the spine and/or sacroiliac joints. Axial spondyloarthritis is one form of spondyloarthritis or spondyloarthropathy, which is a family of rheumatoid conditions where inflammation of the spine and sacroiliac joints is a key distinguishing feature.
Axial spondyloarthritis is an umbrella term that was introduced in 2009 to characterize a diverse disease family that shares clinical and genetic features, such as the involvement of the axial skeleton. The expression was introduced in order to unify (1) less severe forms of spondylitis, (2) the early phase of ankylosing spondylitis as well as (3) ankylosing spondylitis itself into one term.
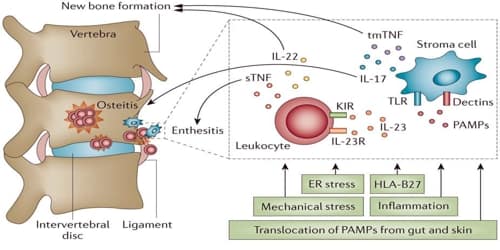
The condition (Axial spondyloarthritis) often affects the bones and joints at the base of the spine where it connects with the pelvis. When the disease is active, these joints become inflamed.
Unlike back pain caused by sports injuries or accidents, axSpA is an inflammatory condition and is generally chronic. People with axSpA can experience periods of painful episodes called ‘flares’, followed by temporary relief.
This type of inflammatory back pain worsens during a period of inactivity – especially at night and early in the morning – and improves with physical activity.
Classification, Causes, and Symptoms of Axial spondyloarthritis:
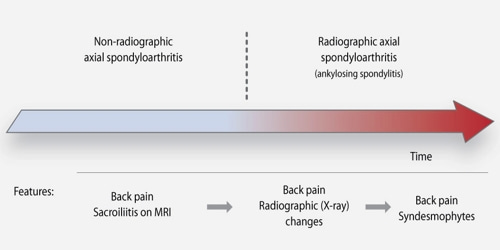
Axial spondyloarthritis can be divided into two classes:
- Non-radiographic axial spondyloarthritis (nr-axSpA): This term encompasses both the early disease stage of ankylosing spondylitis, in which no radiographic changes are visible yet, as well as less severe forms of ankylosing spondylitis.
- Radiographic axial spondyloarthritis: Synonym for ankylosing spondylitis. This class is termed radiographic axial spondyloarthritis due to the unambiguous diagnosis through radiographic changes in the sacroiliac joints and/or spine.
Axial spondyloarthritis causes swelling between the vertebrae, which are the disks that make up the spine, and in the joints between the spine and pelvis. The symptoms can vary but most people experience back pain, stiffness and, in some cases, disability.
The onset of axSpA begins before the age of 40-45, often occurring in the early 20s and 30s.
Symptoms of axSpA can have a major impact on quality of life. The pain and stiffness caused by axSpA can limit the ability to work, socialize and exercise. People with axSpA may also experience:
- psoriasis (irritated, scaly patches of inflamed skin)
- enthesitis (painful inflammation of the tissues that join bone to the muscle)
- dactylitis (swollen fingers and toes)
- inflammatory bowel disease (with abdominal cramping and diarrhea)
- uveitis (eye pain, redness, and sensitivity to light).
Quality of life can be improved if people with axSpA get treatment from rheumatologists, medical specialists who have been trained to diagnose and treat the disease.
Diagnosis and Managment of Axial spondyloarthritis: The disease (Axial spondyloarthritis) is more common and more severe in men. It also often runs in families. The disease has no cure but medicines, exercise, and physiotherapy can relieve the pain, swelling and other symptoms.
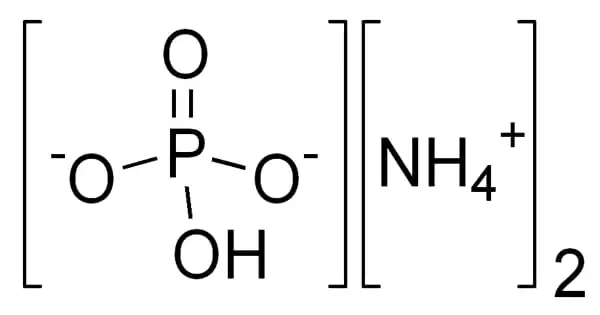
Axial spondyloarthritis is related to the presence of a gene known as HLA-B27. A genetic test for HLA-B27 is available. Along with ankylosing spondylitis, two other types of inflammatory arthritis associated with the presence of HLA-B27 are psoriatic arthritis and enteropathic arthritis.
The problem is that the disease (axSpA) can be mild or it can take years before the x-rays show changes. And even when the x-rays are abnormal, interpretation is always subject to some debate.
Traditional NSAIDs and COX-2 NSAIDs are effective for treating axSpA. The potential harms may not differ when compared to a placebo treatment in the short term. Various NSAIDs are equally effective (e.g.: Cox2 NSAIDS and traditional NSAIDS). Continuous NSAID use may reduce radiographic spinal progression, but this requires confirmation.
Information Source: