Apnea of Prematurity (AOP)
Definition: Apnea of prematurity (AOP) is defined as cessation of breathing by a premature infant that lasts for more than 20 seconds and/or is accompanied by hypoxia or bradycardia. Apnea is traditionally classified as obstructive, central, or mixed. Apnea of prematurity refers to short episodes of stopped breathing in babies who were born before 37 weeks of pregnancy (premature birth).
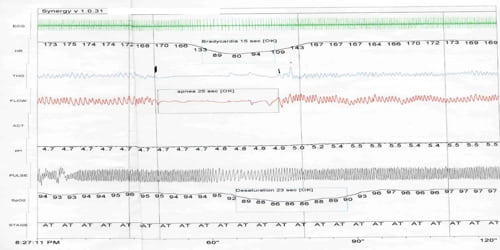
Apnea may be followed by bradycardia, which is a decreased heart rate. When breathing slows, the heart rate also slows. A common term for apnea with bradycardia is “As and Bs.”
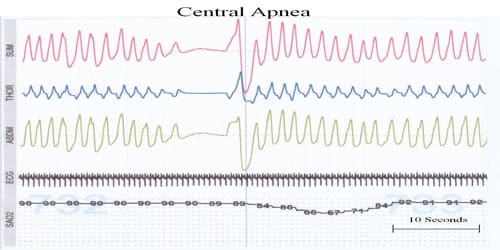
Apnea is classified as central, obstructive, or mixed. Note the following:
- Central apnea is defined as complete cessation of respiration, which can be differentiated from obstructive apnea through a pneumogram, with cessation of airflow and respiratory effort.
- Obstructive apnea is the cessation of airflow in the presence of continued respiratory effort.
- Mixed apnea contains elements of both central and obstructive apnea, either within the same apneic pause or at different times during a period of respiratory recording.
Obstructive apnea may occur when the infant’s neck is hyperflexed or conversely, hyperextended. It may also occur due to low pharyngeal muscle tone or to inflammation of the soft tissues, which can block the flow of air through the pharynx and vocal cords. Central apnea occurs when there is a lack of respiratory effort. This may result from central nervous system immaturity, or from the effects of medications or illness.
Apnea of prematurity usually ends on its own after a few weeks. Once it goes away, it usually doesn’t come back. But no doubt about it — it’s frightening while it’s happening.
Causes and Symptoms of Apnea of prematurity: Apnea of prematurity may be due to a disturbance in the brain’s breathing control center called central apnea. With obstructive apnea, breathing stops because something is blocking the airway. Problems in other organs can also affect the breathing control center. Apnea of prematurity may not have an identifiable cause other than immaturity of the central nervous system.

There are several reasons why newborns, in particular, those who were born early, may have apnea, including:
- If their brain is not fully developed
- If the muscles that keep the airway open are weak
Other stresses in a sick or premature baby may worsen apnea, including:
- Anemia
- Feeding problems
- Heart or lung problems
- Infection
- Low oxygen levels
- Temperature problems
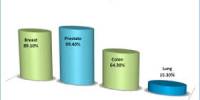
Most babies who develop apnea are premature. It appears to be more common during sleep, especially during active sleep. This is a period when the baby has rapid eye movement (REM) while sleeping. About half of all premature babies have apnea of prematurity.
The breathing pattern of newborns is not always regular and may be called “periodic breathing.” This pattern is even more likely in newborns born early (preemies). Apnea episodes that last longer than 20 seconds are considered serious. The baby may also have a:
- Drop in heart rate. This heart rate drop is called bradycardia or, sometimes, a “brady.”
- Drop in oxygen level (oxygen saturation). This is called desaturation or, sometimes a “desat.”
Apnea is common in premature babies. Most babies have normal outcomes. Mild apnea does not appear to have long-term effects. However, preventing multiple or severe episodes is better for the baby over the long-term.

Diagnosis and Treatment of Apnea of prematurity: Apnea of prematurity (AOP) is fairly common in preemies. Doctors usually diagnose the condition before the mother and baby are discharged from the hospital, and the apnea usually goes away on its own as the infant matures.
AOP can be readily identified from other forms of infant apnea such as obstructive apnea, hypoventilation syndromes, breathing regulation issues during feeding, and reflux-associated apnea with an infant pneumogram or infant apnea/sleep study. It is important to find out if the apnea is due primarily to prematurity or if it is caused by another problem. Diagnostic procedures may include:
- Physical examination
- Blood tests
- Other laboratory tests, such as nasal swabs to check for certain viral infections
- Measurement of the levels of oxygen in the baby’s blood
- X-ray
- Apnea study. This is done to monitor breathing effort, heart rate, and oxygenation.
Generally, babies who are born at less than 35 weeks’ gestation have periods when they stop breathing or their heart rates drop. ‘The medical name for a slowed heart rate is bradycardia.’ These breathing abnormalities may begin after 2 days of life and last for up to 2 to 3 months after the birth. Smaller and more premature infants are more likely to have AOP.
AOP can happen once a day or many times a day. Doctors will closely watch an infant make sure the apnea isn’t due to another condition, such as infection.
- Medications – Methylxanthines (theophylline and caffeine) have been used for almost three decades to treat apnea of prematurity. Despite this prevalent use, there are concerns of long-term negative effects from the use of caffeine. Caffeine and theophylline have similar short-term effects on apnea, but theophylline is associated with higher rates of toxicity.
- Monitoring Breathing – Babies are watched continuously for any sign of apnea. The cardiorespiratory monitor (also known as an apnea and bradycardia, or A/B, monitor) also tracks the infant’s heart rate.
Continuous positive airway pressure. A mechanical breathing machine that pushes a continuous flow of air or oxygen to the airways to help keep tiny air passages in the lungs open.
Since AOP is fundamentally a problem of the immaturity of the physiological systems of the premature infant, it is a self-limited condition that will resolve when these systems mature. It is unusual for an infant to continue to have significant problems with AOP beyond 42 weeks post-conceptual age. There is no evidence that a history of AOP places an infant at increased risk for SIDS. However, any premature infant (regardless of whether they have had AOP) is at increased risk of SIDS. It is important that other factors related to SIDS risk be avoided (exposure to smoking, prone sleeping, excess bedding materials, etc.)
Information Source: