Shortness of Breath
Definition: Shortness of breath (or Breathlessness) is the feeling that one cannot breathe well enough. The medical term for shortness of breath is “dyspnea.” It is often described as an intense tightening in the chest, air hunger or a feeling of suffocation. English dyspnea comes from Latin dyspnoea, from Greek dyspnoia, from dyspnoos, which literally means “disordered breathing”. Its combining forms (dys- + -pnea) are familiar from other medical words, such as dysfunction (dys- + function) and apnea (a- + -pnea).
Shortness of breath is a common symptom. It may be related to serious diseases. It could be a result of being physically out of shape. Medical evaluation should assess if shortness of breath is treatable with lifestyle changes. These include quitting smoking and/or losing weight.
Dyspnea is a normal symptom of heavy exertion but becomes pathological if it occurs in unexpected situations or light exertion. In 85% of cases, it is due to asthma, pneumonia, cardiac ischemia, interstitial lung disease, congestive heart failure, chronic obstructive pulmonary disease, or psychogenic causes, such as panic disorder and anxiety.
If people have unexplained shortness of breath, especially if it comes on suddenly and is severe, see their doctor as soon as possible.

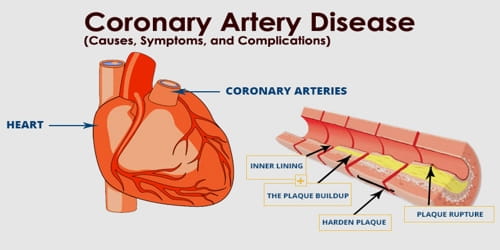
Causes and Risk factors of Shortness of breath: Most causes of shortness of breath are due to heart and lung conditions. Our heart and lungs are involved in transporting oxygen to our body and removing carbon dioxide, and problems with either of these processes affect our breathing.
Shortness of breath that comes on suddenly (called acute) has a limited number of causes, including:
- Asthma (bronchospasm)
- Carbon monoxide poisoning
- Cardiac tamponade (excess fluid around the heart)
- Heart attack
- Heart failure
- Low blood pressure (hypotension)
- Pneumonia (and other pulmonary infections)
- Pneumothorax (collapsed lung)
- Pulmonary embolism (blood clot in an artery in the lung)
- Sudden blood loss
- Upper airway obstruction (blockage in the breathing passage)
The American Thoracic Society defines dyspnea as: “A subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity.” Other definitions describe it as “difficulty in breathing”, “disordered or inadequate breathing”, “uncomfortable awareness of breathing”, and as the experience of “breathlessness” (which may be either acute or chronic).
Risk Factors –
- prior lung diseases
- muscle weakness
- low haemoglobin
- being out of shape from lack of exercise or illness
- severe obesity
- continued exposure to asthma triggers
Smoking is a major risk factor as it causes diseases that result in shortness of breath.
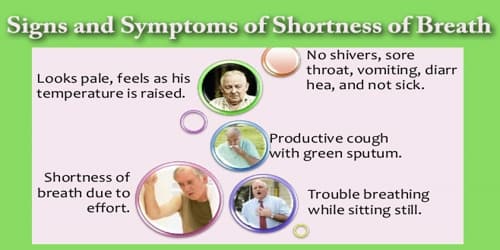
Signs and Symptoms of Shortness of breath: Some people with respiratory problems can feel breathless just by doing normal activities like getting out of a chair or walking to another room. See the medical professional if people’s shortness of breath is accompanied by:
- Swelling in their feet and ankles
- Trouble breathing when they lie flat
- High fever, chills, and cough
- Lips or fingertips turning blue
- Wheezing – abnormal whistling type sound when they breathe in or out
- Stridor – a high pitched noise that occurs with breathing
- Worsening of pre-existing shortness of breath after using their inhalers
- Breathlessness that does not go away after 30 minutes of rest
Some studies have suggested that up to 27% of people suffer from dyspnea (shortness of breath), while dying patients 75% will experience it. Acute shortness of breath is the most common reason people requiring palliative care visit an emergency department.

Diagnosis and Treatment of Shortness of breath: The initial approach to evaluation begins by assessment of the airway, breathing, and circulation followed by a medical history and physical examination. Signs that represent significant severity include hypotension, hypoxemia, tracheal deviation, altered mental status, unstable dysrhythmia, stridor, intercostal indrawing, cyanosis, tripod positioning, and pronounced use of accessory muscles (sternocleidomastoid, scalenes) and absent breath sounds.
Information about the symptoms reported by the patient or other observers is usually sufficient to diagnose shortness of breath. An examination and further tests as noted above may be required. Some patients may need more complex testing including high-resolution CT scans or cardiopulmonary exercise testing.
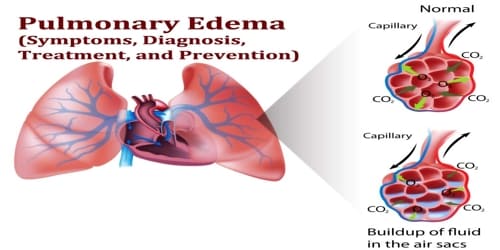
A chest x-ray is useful to confirm or rule out a pneumothorax, pulmonary edema, or pneumonia. Spiral computed tomography with intravenous radiocontrast is the imaging study of choice to evaluate for pulmonary embolism.
The treatment depends on the cause and the duration of symptoms. In those who are not palliative, the primary treatment of shortness of breath is directed at its underlying cause. Extra oxygen is effective in those with hypoxia; however, this has no effect in those with normal blood oxygen saturation, even in those who are palliative.
Shortness of breath can usually be controlled by:
- Medication
- Breathing techniques
- Exercise
- Supplemental oxygen
Other things people can do to prevent and control shortness of breath include:
- Try to not hold the breath
- Using the pursed lips breathing technique
- Sitting in front of a fan, so it blows on the face
- Avoiding triggers that worsen asthma
- Avoiding exposure to pollutants in the air, indoors and outdoors
- Getting a routine health checkup
- Continuing medications as prescribed
- Following an action plan developed with the doctor
- Ensuring the oxygen supply is adequate and the equipment works properly if people rely on supplemental oxygen
Some physical therapy interventions for this population include actively assisted cough techniques, volume augmentation such as breath stacking, education about body position and ventilation patterns and movement strategies to facilitate breathing.
Information Source: