As the COVID-19 vaccination continues to be distributed around the world, many individuals have worries, including if the vaccine impacts antibiotics. Antibiotics taken during the first two years of life can hinder newborns from having a strong immune response to certain immunizations. According to the experts, the new discovery serves as another another warning against overuse of antibiotics.
Babies are inoculated against some infectious diseases throughout their first six months and then receive booster doses in their second year. Antibiotic usage at the time was linked to poor immune responses to four vaccines given to kids to protect them against whooping cough, polio, and other diseases, according to a study published online in Pediatrics.
And the more rounds of antibiotics a youngster took, the lower his or her antibody levels to the immunizations became. With each antibiotic treatment, levels produced by the initial series of vaccinations for the polio, diphtheria-tetanus-pertussis, Haemophilus influenzae type b, and pneumococcal vaccines declined 5 to 11 percent. Antibody levels generated by booster doses of these vaccines declined 12 to 21 percent every course in the children’s second year.
Antibiotics are wonder drugs. This study in no way implies that children who require antibiotics should not receive them. Along with the potential of antibiotic resistance associated with misuse, the effect antibiotics may have on vaccine-induced immunity has therapeutic consequences for every individual kid.
Bali Pulendran
“If anyone needed another reason why antibiotic overuse is bad, this work provides it,” says immunologist Bali Pulendran of Stanford University School of Medicine, who was not involved in the study.
Antibiotic use affects the bacterial population in the gut. That is generally recognized, but researchers are still learning about how that disruption can influence a person’s health. The latest study adds to evidence that reducing the volume and diversity of gut bacteria has an impact on vaccination. Antibiotics inhibited the immune system’s response to vaccines in mouse tests. Furthermore, Pulendran and colleagues showed in 2019 that antibiotics decreased adults’ response to the flu vaccine in those whose prior immunological memory for influenza had weakened.
The study published in Pediatrics is the first to show a link between antibiotic usage and weakened immunization responses in children. Michael Pichichero, a pediatric infectious diseases expert at the Rochester General Hospital Research Institute in New York, and colleagues gathered blood samples from 560 children during normal physician appointments. 342 of those children had been prescribed over 1,700 rounds of antibiotics, while 218 had not received the drugs. The researchers examined whether antibody levels elicited by the four immunizations met the protective threshold and discovered that levels fell short more frequently in children who had received antibiotics.
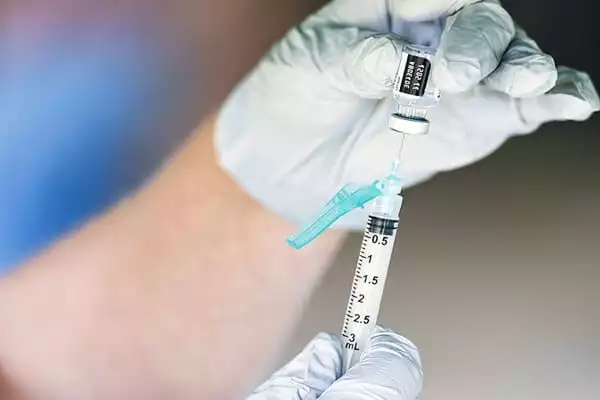
The type and duration of antibiotic treatment also made a difference. Broad-spectrum antibiotics were related with antibody levels below the protective range, whereas a more tailored antibiotic was not. Furthermore, a 10-day course, but not a five-day course, lowered vaccine-induced antibody levels.
The researchers did not investigate whether children in the study with low antibody levels were more likely to develop vaccine-preventable disorders. However, epidemics of whooping cough have happened in the United States despite immunization, according to Pichichero. Perhaps antibiotic use can help explain these outbreaks, he speculates.
Pichichero and colleagues are starting a fresh study with a new set of children to examine what kinds of changes are happening in the gut microbes. Stool samples, blood draws, and antibiotic use records will be collected by the researchers. They’d like to track the children past the age of 5, after they’ve received another round of booster shots, to see if antibiotics interfere with this next chance to acquire antibodies.
Children who are receiving antibiotics for a moderate or severe illness should not be vaccinated until they have recovered – but this applies to all sick children, not just those receiving antibiotics. This is because it might be difficult to determine whether symptoms such as a fever after a vaccination are caused by the vaccine or by the sickness itself. Even if a child is taking antibiotics, he or she can and should receive the vaccine as soon as they feel better.
“Antibiotics are wonder drugs,” says Pichichero. “This study in no way implies that children who require antibiotics should not receive them.” However, he recommends using a precisely focused antibiotic for a shorter course if possible. Along with the potential of antibiotic resistance associated with misuse, the effect antibiotics may have on vaccine-induced immunity “has therapeutic consequences for every individual kid.”