Antibiotic resistance is a major global concern because it reduces antibiotic effectiveness in treating bacterial infections. To address this issue, various strategies are being investigated, including the development of new antibiotics, combination therapies, and alternative treatment approaches.
Researchers report that a drug significantly reduces bacteria’s ability to develop antibiotic resistance in laboratory cultures and animal models, potentially extending antibiotic effectiveness.
A Baylor College of Medicine research team is making progress in their search for solutions to the global problem of bacterial antibiotic resistance, which was responsible for nearly 1.3 million deaths in 2019.
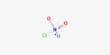
The researchers report in the journal Science Advances on a drug that significantly reduces bacteria’s ability to develop antibiotic resistance in laboratory cultures and animal models, potentially extending antibiotic effectiveness. The drug, known as dequalinium chloride, is a proof-of-concept for drugs that slow evolution.
We discovered that DEQ met both requirements. When combined with cipro, DEQ reduced the development of antibiotic resistance mutations in both laboratory cultures and animal models of infection, and bacteria did not develop resistance to DEQ.
Yin Zhai
“Most people with bacterial infections get better after finishing antibiotic treatment,” said corresponding author Dr. Susan M. Rosenberg, Ben F. Love Chair in Cancer Research and professor of molecular and human genetics, biochemistry and molecular biology, and molecular virology and microbiology at Baylor. She also serves as the program director for the Dan L Duncan Comprehensive Cancer Centre at Baylor.
Rosenberg and her colleagues sought drugs that could prevent or slow the development of E. coli resistance to two antibiotics when exposed to a third antibiotic, ciprofloxacin (Cipro), the second most commonly prescribed antibiotic in the United States and one associated with high bacterial resistance rates.
Resistance is caused by new gene mutations in bacteria that occur during infection. The team discovered that the drug DEQ slows the formation of new mutations in bacteria.

Previous work from the Rosenberg lab had shown that bacterial cultures in the lab exposed to cipro turn up mutation rate. They found a mutational “program” that is switched on by bacterial stress responses. Stress responses are genetic programs that instruct cells to increase the production of protective molecules during stress, including stress from low concentrations of cipro. Low concentrations occur at the beginning and end of antibiotic therapies and if doses are missed.
The same stress responses increase the ability to make genetic mutations, as demonstrated by the Rosenberg group and many other labs. Some of the mutations confer cipro resistance, while others confer resistance to antibiotics not yet encountered. Stress-induced mutation mechanisms are mutation-generating processes that are activated by stress responses.
In the presence of Cipro, bacteria with antibiotic-resistance mutations can sustain an infection. This is the first study to show that bacteria activate a known stress-induced genetic mutational process in animal infections treated with cipro. Cipro resistance is mostly caused by bacteria developing new mutations, both clinically and in the laboratory, rather than acquiring antibiotic resistance genes from other bacteria.
In order to prevent the emergence of antibiotic resistance, the researchers screened 1,120 drugs approved for human use for their ability to reduce the master bacterial stress response, which they demonstrated prevents the emergence of resistance mutations. Furthermore, and counterintuitively, they desired “stealth” drugs that did not slow bacterial proliferation, giving a growth advantage to any bacterial mutants that were resistant to the mutation-slowing drug itself. That is, medications that are not antibiotics in and of themselves.
“We discovered that DEQ met both requirements.” When combined with cipro, DEQ reduced the development of antibiotic resistance mutations in both laboratory cultures and animal models of infection, and bacteria did not develop resistance to DEQ,” said first author Yin Zhai, a postdoctoral associate in the Rosenberg lab. “Moreover, we were able to achieve this mutation-slowing effect at low DEQ concentrations, which is encouraging for patients.” Future clinical trials are required to assess DEQ’s ability to slow bacterial antibiotic resistance in patients.”