Anencephaly
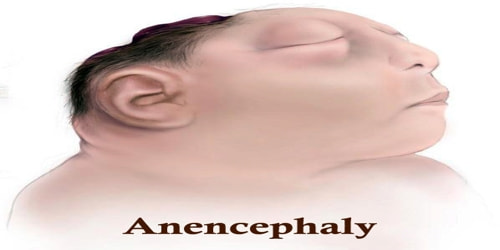
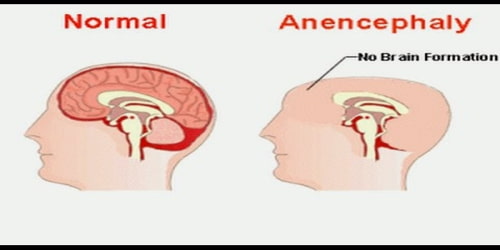
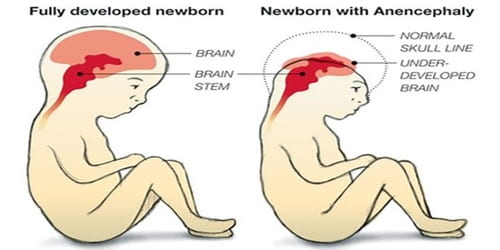
Definition: Anencephaly, also known as “open skull,” is a birth defect in which the major parts of the brain, scalp, and skull of the fetus do not form completely as it is developing in the womb. It is a cephalic disorder that results from a neural tube defect that occurs when the rostral (head) end of the neural tube fails to close, usually between the 23rd and 26th day following conception.
Anencephaly is a type of neural tube defect. It occurs in about 3 of 10,000 pregnancies in the U.S. each year. It is a fatal condition. Infants with anencephaly are stillborn in about 75 percent of cases. The exact number is not known because many of these pregnancies end in miscarriages. This condition most often leads to death in days or weeks.
About one in nearly 5,000 babies is born with anencephaly each year, according to the Centers for Disease Control. The exact number is not known because many pregnancies involving neural tube defects end in miscarriage. More female newborns have anencephaly than males, possibly because of a higher rate of spontaneous abortions or stillbirths among male fetuses.
Causes, Sign, and Symptoms of Anencephaly: The cause of anencephaly is generally unknown, which can be frustrating. For some babies, the cause may be related to a gene or chromosome changes. In most cases, the baby’s parents have no family history of anencephaly.
During pregnancy, the brain and spine begin as a flat plate of cells. This plate rolls into a tube called the neural tube. The tube is completely formed 28 to 32 days after conception. If all or part of the neural tube fails to close, this leaves an opening. The opening is called an open neural tube defect. The opening in the tube may be left exposed. Or it may be covered with bone or skin. Anencephaly is when the neural tube fails to close at the base of the skull.
In about 90 percent of cases, the parents of an anencephalic infant do not have a family history of the disorder. However, if the parents have had a child who was born with anencephaly, they have a greater chance of having another baby with this condition. The recurrence rate for anencephaly is 4 to 5 percent and rises to 10 to 13 percent if the parents have had two other children with anencephaly.
One important risk factor related to anencephaly is inadequate intake of folic acid. A lack of this key nutrient may raise your risk of having a baby with other neural tube defects in addition to anencephaly, such as spina bifida. Pregnant women can minimize this risk with folic acid supplements or diet changes.
The National Institute of Neurological Disorders and Stroke (NINDS) describes the presentation of this condition as follows: “A baby born with anencephaly is usually blind, deaf, unaware of its surroundings and unable to feel pain. Although some individuals with anencephaly may be born with a main brain stem, the lack of a functioning cerebrum permanently rules out the possibility of ever gaining awareness of their surroundings. Reflex actions such as breathing and responses to sound or touch may occur.”
Symptoms can occur a bit differently in each child. They can include:
- No bones on the back of the head
- Missing bones on the front and sides of the head
- Large areas of brain missing
- Folding of the ears
- Split in the roof of the mouth (cleft palate)
- Congenital heart defects
The symptoms of anencephaly can be like other health conditions.
Diagnosis and Treatment of Anencephaly: Anencephaly can often be diagnosed before birth through an ultrasound examination. The maternal serum alpha-fetoprotein (AFP screening) and detailed fetal ultrasound can be useful for screening for neural tube defects such as spina bifida or anencephaly.
Prenatal tests for anencephaly include:
- Blood tests: Tests may show high levels of alpha-fetoprotein, a protein produced by the immature liver cells of the fetus.
- Amniocentesis: A small amount of fluid is withdrawn from the amniotic sac using a long needle that is inserted through the abdomen. The fluid can be analyzed to measure the levels of alpha-fetoprotein and acetylcholinerase. Higher-than-normal levels are linked to neural tube defects, such as anencephaly.
- Ultrasound: This imaging test uses high-frequency sound waves and a computer to make an image (sonogram) of the developing fetus. Abnormalities linked with anencephaly can be seen on the sonogram.
- Fetal MRI: This imaging test uses a magnet to generate an image of the developing fetus. The brain and its various structures can be seen in more detail than the ultrasound alone.
Any of these procedures may be performed between the 14th and 18th weeks of pregnancy. The fetal MRI can be performed at any point of the pregnancy.

There is no treatment or cure for anencephaly. An infant born with the condition should be kept warm and comfortable. If any parts of the scalp are missing, exposed parts of the brain should be covered.
The life expectancy of an infant born with anencephaly is no more than a few days, more likely a few hours.
Four recorded cases of anencephalic children surviving for longer periods of time are Stephanie Keene (better known as Baby K) of Falls Church, Virginia, USA, who lived for 2 years 174 days; Vitoria de Cristo, born in Brazil in January 2010 and surviving until July 17, 2012; Nickolas Coke of Pueblo, Colorado, USA, who lived for 3 years and 11 months, and died October 31, 2012; and Angela Morales, from Providence, Rhode Island, who lived for 3 years and 9 months, and died December 16 2017.
Methods for preventing anencephaly include the following:
- Proper nutrition: Eating nutritious foods and taking a vitamin supplement before and during pregnancy may help prevent neural tube birth defects. Getting enough folic acid is very important. Women of childbearing age should take a daily multivitamin supplement with at least 400 micrograms of folic acid. Other good sources of folic acid include leafy green vegetables, dried beans, oranges, and orange juice. Some products are fortified with folic acid, including enriched flour, rice, bread, pasta, and cereals.
- Folic acid supplements: Pregnant women who have previously given birth to an infant with a neural tube defect may have to take higher amounts of folic acid during pregnancy. It is suggested that women who have had a previous pregnancy involving a neural tube defect should take 4 mg of folic acid, beginning one to two months before conception through their first trimester of pregnancy, under a doctor’s supervision.
Patient’s healthcare provider may also advise genetic counseling. Pregnant women can discuss with a counselor the risk for a neural tube defect in a future pregnancy.
Information Source: