Regenerative heart therapies involve transplanting cardiac muscle cells into damaged parts of the heart to restore function. However, this surgery is apparently associated with a substantial risk of arrhythmias. In a recent study, Japanese researchers tested a unique strategy that involved injecting ‘cardiac spheroids,’ which are produced from human stem cells, directly into injured ventricles. The exceedingly good results reported in primate models illustrate the strategy’s potential.
Cardiovascular illnesses remain among the leading causes of death worldwide, particularly in developed countries. Myocardial infarctions, also known as “heart attacks,” are on the rise and cause a considerable number of deaths each year.
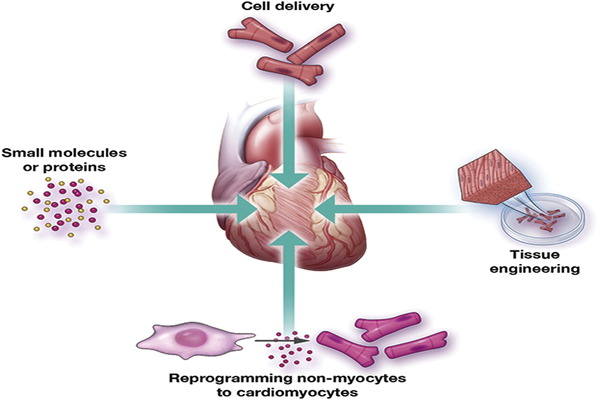
Heart attacks often damage millions of cardiac muscle cells, weakening the heart. Because mammals cannot repair cardiac muscle cells on their own, heart transplants are now the only clinically viable alternative for people who have (or are expected to develop) heart failure. Given the high cost of full heart transplants and the scarcity of donors, it is not surprising that alternative therapies are in high demand among the medical community.
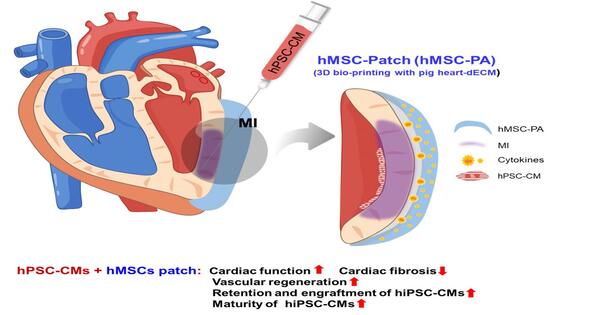
HiPSC-derived cardiac spheroids could potentially serve as an optimal form of cardiomyocyte products for heart regeneration, given their straightforward generation process and effectiveness.
Assistant Professor Kobayashi
One promising strategy that has been steadily gaining traction is using human induced pluripotent stem cells (HiPSCs) for regenerative heart therapy. Simply put, HiPSCs are cells derived from mature cells that can be effectively ‘reprogrammed’ into a completely different cell type, such as cardiac muscle cells (cardiomyocytes). By transplanting or injecting cardiomyocytes derived from HiPSCs into damaged areas of the heart, it is possible to recover some lost functionality. Unfortunately, studies have reported that this approach can increase the risk of arrythmias, posing a major hurdle to clinical trials.
In a recent study, a Japanese research team from Shinshu University and Keio University School of Medicine, tested a new strategy for regenerative heart therapy that involves injecting ‘cardiac spheroids’ derived from HiPSCs into monkeys with myocardial infarction. This study, published on April 26, 2024, in the journal Circulation, was led by Professor Yuji Shiba from the Department of Regenerative Science and Medicine, Shinshu University.
The team included Hideki Kobayashi, the first author, and Koichiro Kuwahara from the Department of Cardiovascular Medicine, Shinshu University School of Medicine, as well as Shugo Tohyama, and Keiichi Fukuda from the Department of Cardiology, Keio University School of Medicine, among others.
The researchers’ unique strategy involved cultivating HiPSCs in a medium that caused them to differentiate into cardiomyocytes. After extracting and purifying cardiac spheroids (three-dimensional clusters of cardiac cells) from cultures, about 6 × 107 cells were injected into the injured hearts of crab-eating macaques (Macaca fascicularis). They kept track of the animals’ health over twelve weeks, collecting regular assessments of heart function. Following that, they examined the monkeys’ hearts at the tissue level to see if cardiac spheroids could restore injured heart muscle.
First, the team verified the correct reprogramming of HiPSCs into cardiomyocytes. They observed, via cellular-level electrical measurements, that the cultured cells exhibited potential patterns typical of ventricular cells. The cells also responded as expected to various known drugs. Most importantly, they found that the cells abundantly expressed adhesive proteins such as connexin 43 and N-cadherin, which would promote their vascular integration into an existing heart.
Afterwards, the cells were transported from the production facility at Keio University to Shinshu University, located 230 km away. The cardiac spheroids, which were preserved at 4 °C in standard containers, withstood the four-hour journey without problem. This means that no extreme cryogenic measures would be needed when transporting the cells to clinics, which would make the proposed approach less expensive and easier to adopt.
Finally, the monkeys were given injections of cardiac spheroids or a placebo straight into the injured heart ventricle. During the observation period, the researchers discovered that arrhythmias were extremely rare, with only two people in the therapy group reporting transitory tachycardia (rapid pulse) in the first two weeks. The team confirmed that the hearts of monkeys that got treatment had better left ventricular ejection after four weeks than the control group, indicating a greater blood pumping capability.
Histological analysis ultimately revealed that the cardiac grafts were mature and properly connected to pre-existing existing tissue, cementing the results of previous observations. “HiPSC-derived cardiac spheroids could potentially serve as an optimal form of cardiomyocyte products for heart regeneration, given their straightforward generation process and effectiveness,” remarks Assistant Professor Kobayashi. “We believe that the results of this research will help solve the major issue of ventricular arrhythmia that occurs after cell transplantation and will greatly accelerate the realization of cardiac regenerative therapy,” he further adds.
Although studied in monkeys, it is important to note that the cardiac spheroid manufacturing methodology used in this study was intended for clinical use in humans. “The positive results acquired thus far are sufficient to provide the green light for our clinical investigation, known as the LAPiS trial. We are already using the same cardiac spheroids on patients with ischemic cardiomyopathy,” says Assistant Professor Kobayashi.
Let us all hope for a resounding success in the LAPiS study, which will pave the way for new and effective treatment options for those suffering from heart disease.