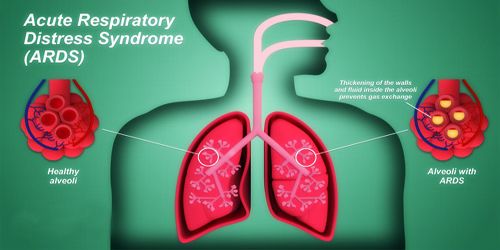
Acute Respiratory Distress Syndrome (ARDS) is a life-threatening condition where the lungs cannot provide the body’s vital organs with enough oxygen. Symptoms include shortness of breath, rapid breathing, and bluish skin coloration. For those who survive, a decreased quality of life is common.
ARDS typically occurs in people who are already critically ill or who have significant injuries. Severe shortness of breath the main symptom of ARDS usually develops within a few hours to a few days after the precipitating injury or infection. Diagnosis is based on a PaO2/FiO2 ratio (ratio of partial pressure arterial oxygen and the fraction of inspired oxygen) of less than 300 mm Hg despite a positive end-expiratory pressure (PEEP) of more than 5 cm H2O. Heart-related pulmonary edema, as the cause, must be excluded.
The primary treatment involves mechanical ventilation together with treatments directed at the underlying cause. Ventilation strategies include using low volumes and low pressures. If oxygenation remains insufficient, lung recruitment maneuvers and neuromuscular blockers may be used. If this is insufficient, extracorporeal membrane oxygenation (ECMO) may be an option. The syndrome is associated with a death rate between 35 and 50%.
Many people who develop ARDS don’t survive. The risk of death increases with age and severity of illness. Of the people who do survive ARDS, some recover completely while others experience lasting damage to their lungs.
Globally, ARDS affects more than 3 million people a year. The condition was first described in 1967. Although the terminology of “adult respiratory distress syndrome” has at times been used to differentiate ARDS from “infant respiratory distress syndrome” in newborns, the international consensus is that “acute respiratory distress syndrome” is the best term because ARDS can affect people of all ages. There are modified diagnostic criteria for children and areas of the world with less resources.
Causes, Sign, and Symptoms of ARDS –
ARDS is primarily caused by damage to the tiny blood vessels in our lungs. Fluid from these vessels leaks into the air sacs of the lungs. These air sacs are where oxygen enters and carbon dioxide is removed from our blood. When these air sacs fill with fluid, less oxygen gets to our blood. Normally, a protective membrane keeps this fluid in the vessels. Severe illness or injury, however, can cause damage to the membrane, leading to the fluid leakage of ARDS.
The most common underlying causes of ARDS include:
- Sepsis – The most common cause of ARDS is sepsis, a serious and widespread infection of the bloodstream.
- Inhalation of harmful substances – Breathing high concentrations of smoke or chemical fumes can result in ARDS, as can inhaling (aspirating) vomit or near-drowning episodes.
- Severe pneumonia – Severe cases of pneumonia usually affect all five lobes of the lungs.
- Head, chest or other major injury – Accidents, such as falls or car crashes, can directly damage the lungs or the portion of the brain that controls breathing.
- Others – Pancreatitis (inflammation of the pancreas), massive blood transfusions and burns.

The signs and symptoms of ARDS often begin within two hours of an inciting event, but can occur after 1–3 days. Signs and symptoms may include shortness of breath, fast breathing, and a low oxygen level in the blood due to abnormal ventilation. Other common symptoms include muscle fatigue and general weakness, low blood pressure, a dry, hacking cough, and fever.
Although most people get ARDS when they’re already in hospital, this is not always the case. It can start quickly as a result of an infection, such as pneumonia, or if someone accidentally inhales their vomit.
Risk Factors and Complications of ARDS –
ARDS is usually a complication of another condition. These factors increase the risk of developing ARDS:
- age over 65 years
- chronic lung disease
- a history of alcohol misuse or cigarette smoking
ARDS can be a more serious condition for people who:
- have toxic shock
- are older
- have liver failure
- have a history of alcohol misuse
Because ARDS is often caused by a serious health condition, about 1 in 3 people who get it will die. But most deaths are the result of the underlying illness, rather than ARDS itself. For those who survive, the main complications are linked with nerve and muscle damage, which causes pain and weakness. Some people also develop psychological problems, such as post-traumatic stress disorder (PTSD) and depression. The lungs usually recover and long-term lung failure after ARDS is rare.
Diagnosis and Treatment of ARDS –
There’s no specific test to diagnose ARDS. A full assessment is needed to identify the underlying cause and rule out other conditions.
The assessment is likely to include:
- a physical examination
- blood tests to measure the amount of oxygen in the blood and check for an infection
- a pulse oximetry test, where a sensor attached to your fingertip, ear or toe is used to measure how much oxygen your blood is absorbing
- a chest X-ray and a CT scan to look for evidence of ARDS
- an echocardiogram – a type of ultrasound scan that’s used to look at your heart and nearby blood vessels.

Acute respiratory distress syndrome is usually treated with mechanical ventilation in the intensive care unit (ICU). Mechanical ventilation is usually delivered through a rigid tube which enters the oral cavity and is secured in the airway (endotracheal intubation), or by tracheostomy when prolonged ventilation (≥2 weeks) is necessary. The role of non-invasive ventilation is limited to the very early period of the disease or to prevent worsening respiratory distress in individuals with atypical pneumonias, lung bruising, or major surgery patients, who are at risk of developing ARDS. Treatment of the underlying cause is crucial. Appropriate antibiotic therapy is started as soon as culture results are available, or if infection is suspected (whichever is earlier). Empirical therapy may be appropriate if local microbiological surveillance is efficient. Where possible the origin of the infection is removed. When sepsis is diagnosed, appropriate local protocols are followed.
People with ARDS are often given medication to deal with side effects. These include the following types of medications:
- pain medication to relieve discomfort
- antibiotics to treat an infection
- blood thinners to keep clots from forming in the lungs or legs
- If you’re recovering from ARDS, the following suggestions can help protect your lungs:
- Quit smoking. If you smoke, seek help to quit, and avoid secondhand smoke whenever possible.
- Get vaccinated. The yearly flu (influenza) shot, as well as the pneumonia vaccine every five years, can reduce your risk of lung infections.
People recovering from ARDS may need pulmonary rehabilitation. This is a way to strengthen the respiratory system and increase lung capacity. Such programs can include exercise training, lifestyle classes, and support teams to aid in recovery from ARDS.
As of 2019, there is no evidence showing that treatments with exogenous surfactants, statins, beta-blockers or n-acetylcysteine decreases early mortality, late all-cause mortality, duration of mechanical ventilation, or number of ventilator-free days. The overall prognosis of ARDS is poor, with mortality rates of approximately 40%.
Preventions of ARDS –
There’s no way to prevent ARDS completely. However, people may be able to lower their risk of ARDS by doing the following:
- Seek prompt medical assistance for any trauma, infection, or illness.
- Stop smoking cigarettes, and stay away from secondhand smoke.
- Give up alcohol. Chronic alcohol use may increase your mortality risk and prevent proper lung function.
- Get your flu vaccine annually and pneumonia vaccine every five years. This decreases your risk of lung infections.
Recovery from ARDS can be a long road, and people will need plenty of support. Although everyone’s recovery is different, being aware of common challenges encountered by others with the disorder can help.
Information Sources: