According to a groundbreaking paper authored by a team led by The University of Texas Health Science Center at San Antonio, also known as UT Health San Antonio, a typical Western high-fat diet can increase the risk of painful disorders common in people with conditions such as diabetes or obesity.
Furthermore, dietary changes may significantly reduce or even reverse pain caused by conditions that cause either inflammatory pain (arthritis, trauma, or surgery) or neuropathic pain (diabetes). The novel discovery could aid in the treatment of chronic pain patients by simply changing their diet or developing drugs that block the release of certain fatty acids in the body.
A collaborative team of 15 local researchers, led by first co-authors Jacob T. Boyd, MD, Ph.D., and Peter M. LoCoco, Ph.D., of the Department of Endodontics at UT Health San Antonio, published the paper, which had been in the works for more than five years, in the June edition of the journal Nature Metabolism.
A typical Western high-fat diet can increase the risk of painful disorders common in people with conditions such as diabetes or obesity, according to a new study.
Eleven of the co-authors are from UT Health San Antonio, including seven current or former Graduate School of Biomedical Sciences students; three are from the University of Texas at San Antonio’s Department of Chemistry, and one is from the South Texas Veterans Health Care System’s Department of Neurology.
“This study exemplifies team science at its best,” said Kenneth M. Hargreaves, DDS, Ph.D., professor, and chair of the Department of Endodontics at UT Health San Antonio and senior author of the paper.
An estimated 20.4 percent of adults in the United States suffer from chronic pain, with those 65 and older being the most likely to report suffering from the condition. While many medications aim to alleviate the burden of chronic pain once it has developed, new research suggests that there may be a way to reduce your chronic pain risk—all it takes is a few dietary changes.

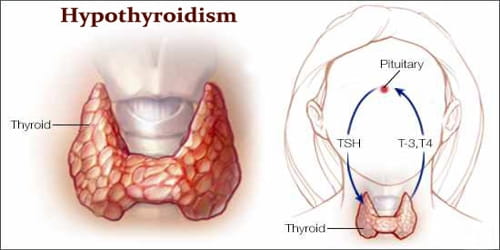
Fatty acids and pain
Chronic pain is a leading cause of disability worldwide. However, while dietary lipids, or fatty acids, are frequently recommended to manage diabetes, auto-immune disorders, and cardiovascular disease, the role of dietary lipids, or fatty acids, in pain conditions is relatively unknown.
Dr. Boyd and his colleagues used a variety of methods in both mice and humans to investigate the role of polyunsaturated fatty acids in pain conditions in their new paper. They discovered that eating a typical Western diet high in omega-6 polyunsaturated fats was a significant risk factor for both inflammatory and neuropathic pain.
Omega-6 fats, which are mostly found in foods containing vegetable oils, have health benefits. However, Western diets associated with obesity have much higher levels of those acids in foods ranging from corn chips to onion rings than healthy omega-3 fats found in fish and sources such as flaxseed and walnuts.
Processed snacks, fast foods, cakes, and fatty and cured meats are all examples of unhealthy foods high in omega-6 fats. The researchers discovered that reversing this diet, particularly by lowering omega-6 and increasing omega-3 lipids, significantly reduced these pain conditions. Furthermore, the authors demonstrated that skin omega-6 lipid levels in patients with Type 2 diabetic neuropathic pain were strongly related to reported pain levels and the need for analgesic drugs.
“This paper is a high-profile contribution for a huge unmet translational need because there are no treatments altering the nature of this neurological disease,” said José E. Cavazos, MD, Ph.D., professor of neurology, assistant dean, and director of the South Texas Medical Scientist Training Program at UT Health San Antonio, which is funded by the National Institutes of Health.
Duke University researchers Aidan McGinnis and Ru-Rong Ji wrote in an accompanying editorial, “This comprehensive and elegant study from Boyd et al. may serve as a foundation for new clinical trials and ultimately provide new avenues for the clinical treatment of neuropathies.”