Genome sequencing revealed a significant surprise a decade ago: mutations in epigenetic regulators, which govern gene activity, are connected to nearly half of all human malignancies.
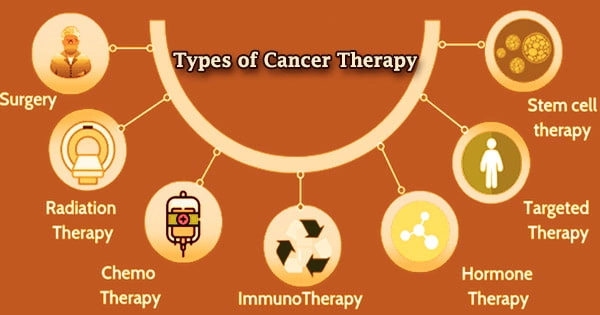
The treatment of cancer in a patient with surgery, chemotherapy, and/or radiation is known as cancer therapy. For some cancer forms, targeted therapy are also available. A cancer patient may get a variety of treatments, including ones aimed at alleviating cancer symptoms such as pain.
A team of scientists led by Oliver Bell of USC and Stephen V. Frye of the University of North Carolina at Chapel Hill developed a new drug-like molecule that can counteract the effects of mutated epigenetic regulators, which are known to drive certain types of cancer, including lymphoma, according to a new study published in Cell Chemical Biology.
How epigenetic regulators control gene activity
Epigenetic regulators play a critical function in healthy cells, turning on and off hundreds of genes in a well-coordinated sequence that regulates normal human development. One of these epigenetic regulators, EZH2, regulates the transitory inactivation of particular genes to allow immune cells to mature.
Mutated EZH2, on the other hand, may induce continuous suppression of these genes, preventing immune cells from growing properly and eventually transforming them into malignant tumors. Some cancer patients will just require one therapy. Most patients, on the other hand, receive a mix of therapies, such as surgery combined with chemotherapy and/or radiation therapy.
The good news is that, unlike many other types of mutations, cancer-causing mutations in epigenetic regulators may be reversible with treatment. With this in mind, first author Junghyun L. Suh and the research team set out to create a drug-like chemical that may reverse EZH2’s inhibition of cancer-causing genes.
When we exposed human lymphoma and colorectal cancer cells to our newly synthesized drug-like molecule in the laboratory, the malignant cells ceased to proliferate and began to behave more like healthy cells.
Oliver Bell
The role of “writers” and “readers”
Suh and her colleagues began by looking at the mechanism through which EZH2 regulates gene repression. EZH2 functions as a “writer,” indicating which genes will be suppressed. CBX8, a second epigenetic regulator, acts as a “reader,” interpreting the repressive marks and recruiting further regulatory machinery to turn the genes off.
In comparison to the writer, the reader CBX8 appears to be similarly important for cancer cell proliferation but less so for healthy cell function. This means that medications that target the reader are more likely to have less damaging side effects on the patient’s healthy cells.
To target CBX8, the researchers first created mouse stem cells that allowed them to quickly test a huge number of drug-like compounds. CBX8 read the markers left by EZH2 to suppress a gene that produces a detectable green fluorescent protein (GFP) in these modified stem cells. The scientists recognized that a drug-like chemical had successfully stopped CBX8 from reading the repressive tags if the stem cells exhibited activation of the characteristic green light.
Targeting the “reader” to counteract the mutation
The researchers then used their understanding of CBX8 to create numerous iterations of drug-like compounds that were specifically targeted at this reading. CBX’s complex protein structure, as well as how it binds to DNA and reads repressive tags, were all taken into account.
They went on to testing in human cancer cells after producing a powerful chemical that functioned well in the modified mice cells.
“When we exposed human lymphoma and colorectal cancer cells to our newly synthesized drug-like molecule in the laboratory, the malignant cells ceased to proliferate and began to behave more like healthy cells,” said the study’s co-corresponding author Oliver Bell, who is an assistant professor of biochemistry and molecular medicine, and stem cell biology and regenerative medicine at the Keck School of Medicine of USC, and a member of the USC Norris Comprehensive Cancer Center.
“Our CBX8-targeted molecule has the most powerful effect that we’ve seen so far in terms of blocking the reader’s function,” added co-corresponding author Stephen V. Frye, who is the Fred Eshelman Distinguished Professor and Co-director of the Center for Integrative Chemical Biology and Drug Discovery at the University of North Carolina at Chapel Hill.
“This paves the way for further research into relevant cancer medicines, as well as a better knowledge of epigenetic control in normal human development.”