A Michigan Medicine study suggests that researchers have discovered a novel, non-invasive way to measure blood flow to the brains of newborn children at the bedside – a method that has the potential to improve diagnosis and treatment across medicine.
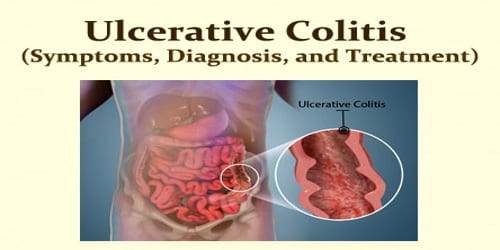
When a fetus develops, fluid fills the baby’s lungs, and oxygen is delivered directly from the placenta. This oxygenated blood bypasses the lungs and travels to the rest of the body via a vessel known as the ductus arteriosus.
After birth, babies use their lungs to breathe, and the ductus arteriosus typically closes within several days. But for nearly 65% of pre-term infants, the vessel fails to close. This condition called patent ductus arteriosus, or PDA, shifts blood flow into an abnormal path which can strain the heart, congest the lungs and steal blood and oxygen from the newborn baby’s brain and other organs.
Physicians must decide whether to attempt to close the PDA with medications or an implanted device, both of which have risks. Accurately measuring blood flow to the newborn’s organs could help with this important decision. But an issue arises: there is no true blood flow measurement that practically works for clinical use, said Jonathan Rubin, M.D., Ph.D., professor emeritus of radiology at the University of Michigan Medical School.
There are several other methods of measuring blood flow, but they are cumbersome and often require intravenous contrast agents, with babies being sedated or restrained in a scanner. But pre-term babies are in incubators; they are fragile, and these techniques can be dangerous. This ultrasound technique could be used routinely in neonatal intensive care units, which could significantly impact outcomes for pre-term babies with this condition.
Jonathan Rubin
“This decision about whether to close the patent ductus arteriosus has been an issue in neonatology for at least 30 years,” Rubin said. “The debate really hangs on how the blood flow has shifted, complicated by a history of unreliable data, which is why a measurement of blood flow is so important.”
To address this problem, Rubin and a team of researchers at Michigan Medicine developed a real-time ultrasound color flow technique that relies on 3D sampling to measure blood flow. They tested the method on 10 healthy, full-term babies, obtaining total brain blood flow measurements that closely match those using more invasive or technically demanding techniques. The results are published in Ultrasound in Medicine and Biology.
“With our method, we are able to scan babies in the parent’s arms with no pain or danger – nobody has really been able to do that before,” said Rubin, a lead author of the paper.
“There are several other methods of measuring blood flow, but they are cumbersome and often require intravenous contrast agents, with babies being sedated or restrained in a scanner. But pre-term babies are in incubators; they are fragile, and these techniques can be dangerous. This ultrasound technique could be used routinely in neonatal intensive care units, which could significantly impact outcomes for pre-term babies with this condition.”

How it works
There are many surrogate methods used in lieu of true blood flow, such as blood flow velocity. But true blood flow requires knowing the velocity of the blood in relation to the area it covers.
Like traffic, Rubin says, it doesn’t help to only know how fast cars are moving if you don’t know how many cars are on the road.
The technique developed by Rubin and his colleagues measures true blood flow by calculating blood flow flux over a surface across ultrasound beams. The color image is captured in 3D.
“This method does not require contrast agents, measurements can be performed in real-time, and they can be repeated as needed since the method is totally benign,” Rubin said.
Game-changing applications
With a non-invasive, true measure of blood flow, researchers say the technique could be applied to address blood flow to organs including the brain, the liver, and kidneys in many disease states including congestive heart failure, sepsis, and shock.
“In the Neonatal Intensive Care Unit, we must make assumptions every day based on indirect measures to determine how our treatments affect blood flow to the organs of critically ill newborns,” said Gary Weiner, M.D., clinical associate professor of pediatrics at U-M Medical School and medical director of the Brandon Neonatal Intensive Care Unit at U-M Health C.S. Mott Children’s Hospital.
“Having a safe, rapid, accurate bedside tool that allows us to measure true blood flow could be a game changer.”
But it doesn’t stop with children. Rubin says the method has the potential to be applied almost anywhere an ultrasound can image, being used for anything from assessing need for organ transplants to identifying issues during surgical procedures.
“Clinicians perform all kinds of maneuvers to modify blood flow measurements, and the assessments are always semi-quantitative or make unjustified assumptions about the nature of the flow,” he said. “They may use a Doppler ultrasound to get velocity, but then just feel a vessel to feel if there is flow. There is so much potential for this application in diagnostic medicine because flow is everywhere. We have already used the method to measure flows in umbilical cords in fetuses before birth and in livers in adults. The method is being evaluated by several companies for inclusion on standard clinical ultrasound scanners.”