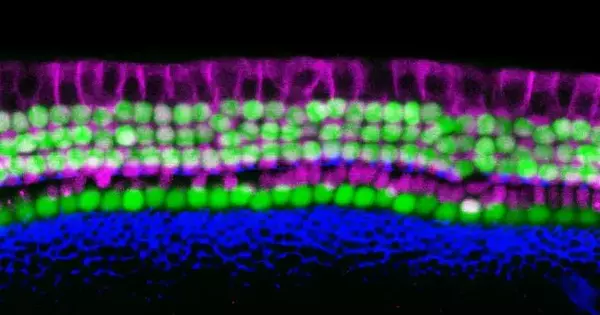
Because mammalian inner ear hair cells do not regenerate on their own, irreversible damage is the primary cause of sensorineural hearing loss. Hair cell damage and loss are primarily caused by factors such as aging, infection, genetic factors, hypoxia, autoimmune diseases, ototoxic drugs, or noise exposure. In recent years, research on the regeneration and functional recovery of mammalian auditory hair cells has gotten a lot of attention in the field of auditory research.
Neil Segil and Justin Ichida of the USC Stem Cell laboratories are whispering the secrets of a simpler way to generate inner ear sensory cells. Their method employs direct reprogramming to generate sensory cells known as “hair cells” because of their hair-like protrusions that detect sound waves. The findings were published in the journal eLife.
“We’ve succeeded in directly reprogramming a variety of mouse cell types into what we’re calling induced hair cell-like cells, or iHCs,” said lead author and Ph.D. student Louise Menendez. “This enables us to generate a large number of iHCs in a timely manner in order to identify causes and treatments for hearing loss.”
In the short term, researchers can use iHCs to screen a large number of drug candidates that could prevent or treat hearing loss. In the future, it may be possible to directly reprogram supporting cells in a deaf person’s inner ear as a way to restore hearing.
Louise Menendez
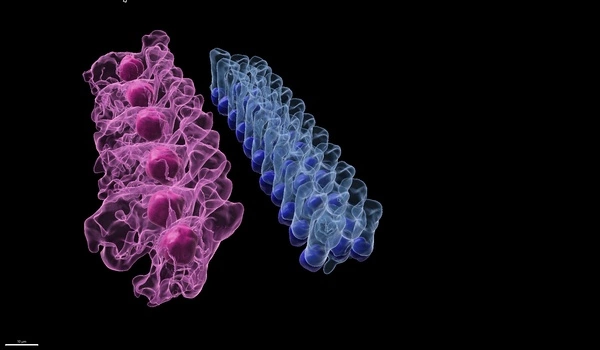
The researchers successfully reprogrammed three different types of mouse cells to become iHCs. The first two types were embryonic and adult versions of connective tissue cells known as fibroblasts. The third was a different type of inner ear cell known as a supporting cell.
To achieve reprogramming, the scientists exposed fibroblasts and supporting cells to a cocktail of four transcription factors, which are molecules that aid in the transmission of DNA instructions. The cocktail was discovered by testing various combinations of 16 transcription factors that were highly active in the hair cells of newborn mice.
“The four key ingredients turned out to be the transcription factors Six1, Atoh1, Pou4f3, and Gfi1,” said Menendez.
The resulting iHCs resembled naturally occurring hair cells in terms of their structure, electrophysiology, and genetic activity. The iHCs also possessed several other distinct characteristics of hair cells, including vulnerability to an antibiotic known to cause hearing loss.
“Hair cells are easy to damage and currently impossible to repair in humans,” said Segil, a professor in the USC Tina and Rick Caruso Department of Otolaryngology — Head and Neck Surgery and one of the study’s corresponding authors. “Aging, loud noises, and certain chemotherapy drugs and antibiotics can all cause permanent loss of hair cells, which is the leading contributor to hearing loss worldwide.”
iHCs have the potential to accelerate hearing loss research in at least two important ways, according to Ichida, who is the John Douglas French Alzheimer’s Foundation Associate Professor of Stem Cell Biology and Regenerative Medicine at USC, and the other corresponding author of the study.
Neural stem cells have the ability to self-renew and differentiate into different types of nerve cells, making them a potential treatment for a variety of diseases. Some supporting cells with the ability to proliferate in the inner ear are also known as sensory precursor cells. When an organism’s normal structure is damaged or changed, stem cell therapy is a treatment that uses the diversity of stem cells to induce differentiation into the same structure as the original shape and function. This treatment can help to replace the damaged and defective inner ear hair cells.
“In the short term, researchers can use iHCs to screen a large number of drug candidates that could prevent or treat hearing loss,” said Ichida, a New York Stem Cell Foundation-Robertson Investigator. “In the future, it may be possible to directly reprogram supporting cells in a deaf person’s inner ear as a way to restore hearing.”