The excellent findings of a clinical study for liraglutide, a frequently prescribed weight-loss medication, were revealed by researchers at UT Southwestern. Once-daily liraglutide paired with lifestyle changes effectively reduced two kinds of fat that have been associated with danger to heart health: visceral fat and ectopic fat, in individuals who are overweight or have obesity along with high cardiovascular risk.
“Our study used the latest imaging technology to evaluate different fat components in the body. The main finding was a significant decrease in visceral fat in patients without diabetes but who were overweight or had obesity. These results show the potential of liraglutide treatment for significantly lowering the risk of chronic disease in this population,” said Parag Joshi, M.D., preventive cardiologist, Assistant Professor of Cardiology, and senior author of the study published in The Lancet Diabetes & Endocrinology.
Overweight people have a Body Mass Index (BMI) between 25 and 30. Obesity is characterized as a body mass index (BMI) of 30 or above. Prescription medicines for the treatment of obesity and overweight operate in a variety of ways.
The key to losing weight is to burn more calories than you consume. You may do this by consuming less calories from foods and beverages while increasing the number of calories expended via physical exercise. Your doctor may recommend weight-loss surgery or medicines if you have significant health problems as a result of your weight.
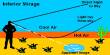
Visceral fat is deposited around vital internal organs including the liver, pancreas, and intestines in the abdominal cavity. Ectopic fat is deposited in organs including the liver, skeletal muscle, heart, and pancreas that typically contain tiny quantities of fat.
Over the course of 40 weeks, the 185 research participants were given a once-daily injection of liraglutide. Liraglutide had two-fold larger fat-burning effects in the abdominal tissues and six-fold more fat-burning effects in the liver than it did on overall body weight.
Weight-loss medicines are designed to assist people who are overweight or obese and are experiencing health concerns as a result. BMI is a metric used by doctors to determine whether you could benefit from weight-loss drugs.
The treatment impact was consistent across race/ethnicity, BMI categories, and whether people had or didn’t have prediabetes at the start. Liraglutide also decreased fasting blood glucose and inflammation in people without diabetes who had normal blood sugar levels at the start of the study.
The rate of the first occurrence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke among patients with type 2 diabetes was lower in those treated with liraglutide than in those treated with placebo in a 2016 study led by UTSW investigators called the Leader trial.
Symptoms of type 2 diabetes can develop over a period of years and go unnoticed for a long time (in rare cases, there are no symptoms at all). Symptoms often appear gradually. Heart disease, strokes, diabetic retinopathy, which can lead to blindness, renal failure, and poor blood flow in the limbs, which can lead to amputations, are all long-term consequences of high blood sugar. Ketoacidosis is rare, although rapid development of the hyperosmolar hyperglycemic condition is possible.
“Our findings help add a possible mechanism for why there is a benefit of liraglutide on cardiovascular outcomes while also showing its benefits in people without diabetes,” said Dr. Joshi.
Obesity affects one out of every four adults and one out of every five children, according to the study, putting them at a higher risk of cardiovascular disease and death. “Excess visceral fat and ectopic (e.g., liver) fat are central to the development of type 2 diabetes and cardiovascular disease,” said Dr. Joshi. “It’s still difficult to identify people who are most at risk and provide them with therapy in addition to lifestyle modifications like diet and exercise.”
Novo Nordisk provided funding for the study through an investigator-initiated grant. Colby R. Ayers, Bienka Lewis, Robert Oslica, Susan Rodder, and Ambarish Pandey are among the UT Southwestern scholars that contributed to the study.