A nano drug, also known as a nanomedicine, is a type of drug delivery system that uses nanotechnology to improve the efficacy and safety of drugs. Nanomedicine refers to the application of nanotechnology to the development of medical devices and drugs.
Using nanoparticles, researchers at the Masonic Medical Research Institute have found a novel technique to treat pulmonary fibrosis, a degenerative, incurable condition that causes the lungs to harden through scarring.
“While these findings do not yet necessarily cure this disease outright, it shows we have the potential to dramatically impact and improve the quality of life for those affected,” said the study’s senior investigator, Jason R. McCarthy, Ph.D., Associate Professor and Science Operations Director at MMRI.
Dr. McCarthy along with 15 collaborators on this project, which include scientists from the MMRI, Massachusetts General Hospital, and Harvard Medical School, embarked upon this study in 2015. The American Journal of Physiology-Lung Cellular and Molecular Physiology published its findings earlier this year.
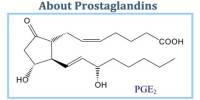
The idea behind the study was not to find a novel therapeutic, per se, but to look at whether delivering effective known drugs to specific cells in the lung can have a more potent therapeutic effect,” Dr. McCarthy said. “What we showed is that it is indeed possible to target a drug to diseased cells to interrupt the process of cell death and scarring.
Professor Jason R. McCarthy
The group concentrated on creating nanoparticles that could specifically target lung fibroblasts, the type of cell that causes scarring, in order to deliver a potent medication that would stop the disease’s progression.
“The idea behind the study was not to find a novel therapeutic, per se, but to look at whether delivering effective known drugs to specific cells in the lung can have a more potent therapeutic effect,” Dr. McCarthy said. “What we showed is that it is indeed possible to target a drug to diseased cells to interrupt the process of cell death and scarring.”
In order to better understand how certain cell types work or malfunction during idiopathic pulmonary fibrosis, Dr. McCarthy and his team are currently examining if this approach could also be beneficial for other lung cell types.
Similar to this, they are extending their research to look at how this tactic might be used in other organ systems, such as the heart and liver, in addition to the lung.