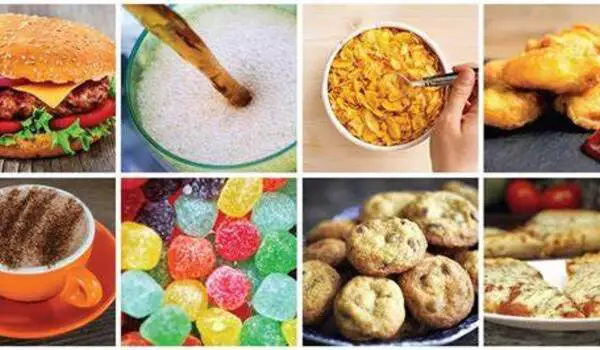
According to a new study led by researchers from the University of Bristol and the International Agency for Research on Cancer (IARC), eating more ultra-processed foods (UPFs) may be associated with an increased risk of developing cancers of the upper aerodigestive tract (including the mouth, throat, and esophagus). Obesity associated with UPF consumption may not be the only factor to blame, according to the authors of this international study, which analyzed diet and lifestyle data on 450,111 adults who were followed for approximately 14 years. The findings have been published in the European Journal of Nutrition.
Several studies have found a link between UPF consumption and cancer, including a recent study that looked at the link between UPFs and 34 different cancers in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort, Europe’s largest cohort study.
As more evidence emerges about the links between eating UPFs and negative health outcomes, researchers from Bristol Medical School and IARC wanted to dig deeper. Because many UPFs have an unhealthy nutritional profile, the researchers wanted to see if the link between UPF consumption and head and neck cancer and esophageal adenocarcinoma (esophageal cancer) in EPIC could be explained by an increase in body fat.
This study adds to a growing pool of evidence suggesting a link between UPFs and cancer risk. The link between UPF consumption and an increased risk of developing upper-aerodigestive tract cancer backs up our Cancer Prevention Recommendations to eat a healthy diet rich in wholegrains, vegetables, fruit, and beans.
Dr Helen Croker
Results from the team’s analyses showed that eating 10% more UPFs is associated with a 23% higher risk of head and neck cancer and a 24% higher risk of esophageal adenocarcinoma in EPIC. Increased body fat only explained a small proportion of the statistical association between UPF consumption and the risk of these upper-aerodigestive tract cancers.
Fernanda Morales-Berstein, a Wellcome Trust PhD student at the University of Bristol and the study’s lead author, explained: “UPFs have been associated with excess weight and increased body fat in several observational studies. This makes sense, as they are generally tasty, convenient and cheap, favouring the consumption of large portions and an excessive number of calories. However, it was interesting that in our study the link between eating UPFs and upper-aerodigestive tract cancer didn’t seem to be greatly explained by body mass index and waist-to-hip ratio.”
The authors suggest that other mechanisms could explain the association. For example, additives including emulsifiers and artificial sweeteners which have been previously associated with disease risk, and contaminants from food packaging and the manufacturing process, may partly explain the link between UPF consumption and upper-aerodigestive tract cancer in this study.
However, Fernanda Morales-Berstein and colleagues cautioned about their findings, suggesting that the associations found in the study between UPF consumption and upper-aerodigestive tract cancers could be influenced by certain types of bias. This explains why they discovered evidence of a link between higher UPF consumption and an increased risk of accidental death, which is highly unlikely to be causal.
George Davey Smith, Professor of Clinical Epidemiology and Director of the MRC Integrative Epidemiology Unit at the University of Bristol, and co-author on the paper, said: “UPFs are clearly associated with many adverse health outcomes, yet whether they actually cause these, or whether underlying factors such as general health-related behaviours and socioeconomic position are responsible for the link, is still unclear, as the association with accidental deaths draws attention to.”
Inge Huybrechts, Team head of the Lifestyle exposures and interventions team at IARC, added: “Cohorts with long-term dietary follow-up intake assessments, considering also contemporary consumption habits, are needed to replicate these study’s findings, as the EPIC dietary data were collected in the 1990s, when the consumption of UPFs was still relatively low. As such associations may potentially be stronger in cohorts including recent dietary follow-up assessments.”
More research is needed to identify other mechanisms, such as food additives and contaminants, that could explain the observed links. However, based on the finding that body fat did not explain much of the link between UPF consumption and upper-aerodigestive tract cancer risk in this study, Fernanda Morales-Berstein suggested that “focusing solely on weight loss treatment, such as Semaglutide, is unlikely to greatly contribute to the prevention of upper-aerodigestive tract cancers related to eating UPFs.”
“This study adds to a growing pool of evidence suggesting a link between UPFs and cancer risk,” said Dr Helen Croker, Assistant Director of Research and Policy at World Cancer Research Fund. The link between UPF consumption and an increased risk of developing upper-aerodigestive tract cancer backs up our Cancer Prevention Recommendations to eat a healthy diet rich in wholegrains, vegetables, fruit, and beans.”