One of the most prevalent types of dementia, dementia with Lewy bodies (DLB), has no known cure. Nevertheless, the bacteria responsible for DLB had not been found. Earlier research had suggested that gut bacteria, or the germs that reside in the human digestive tract, may have a role in Parkinson’s disease, another neurodegenerative ailment.
Now, a group led by researchers at the Nagoya University Graduate School of Medicine in Japan has identified three bacteria involved in DLB: Collinsella, Ruminococcus, and Bifidobacterium. Their research, which was published in the journal Parkinson’s Disease, offers novel diagnostic and therapeutic options.
An aberrant buildup of the brain protein alpha-synuclein, which is involved in signal transmission between neurons, is linked to the start of DLB. These deposits, also referred to as “Lewy bodies,” alter the chemistry in the brain, impairing thinking, reasoning, and memory. Confusion, memory loss, slowed movement, and visual hallucinations are among the symptoms.
Parkinson’s disease also begins with movement issues, but after a year, some sufferers start to lose cognitive function. When significant cognitive deterioration happens, these patients are identified as having DLB. It is challenging for doctors to anticipate which Parkinson’s disease patients may have cognitive deterioration within a year and acquire DLB.
A research group led by Associate Professor Masaaki Hirayama (Omics Medicine), Professor Kinji Ohno (Neurogenetics), and Assistant Professor Hiroshi Nishiwaki (Neurogenetics) of Nagoya University Graduate School of Medicine, in collaboration with Okayama Neurology Clinic, Iwate Medical University, and Fukuoka University, analyzed microorganisms in the gut and fecal bile acids of patients with DLB, Parkinson’s disease, and rapid eye movement behavior disorder.
Our findings can be used both for both diagnosis and treatment. If a patient with Parkinson’s disease develops dementia in one year after the onset of motor symptoms, they are diagnosed with DLB. However, we cannot currently predict whether a patient with Parkinson’s disease will become a DLB patient. The gut microbiome will help to identify such patients.
Professor Kinji Ohno
They found that patients with DLB were associated with three gut bacteria, Collinsella, Ruminococcus, and Bifidobacterium. This may point to potential diagnostic and therapeutic approaches for this neurodegenerative condition.
The gut bacteria associated with DLB and Parkinson’s disease share certain similarities, according to the study. The intestinal mucosa-degrading bacterium Akkermansia increased in both illnesses. On the other hand, there was a decline in the number of short-chain fatty acid (SCFA)-producing bacteria in the stomach.
“Decreases in SCFA-producing bacteria have been repeatedly reported in Parkinson’s disease, Alzheimer’s disease, and ALS,” explains Ohno. “This suggests that it is a common feature of neurodegenerative diseases.”
SCFA are important because they produce regulatory T cells. These types of cells play a critical role in regulating the immune system by suppressing neuroinflammation.
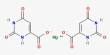
In contrast, the researchers discovered an increase in Ruminococcus torques, an increase in Collinsella, and a decrease in Bifidobacterium in patients with DLB. Those with Parkinson’s disease experienced a shift in their levels, which was distinct from this. With the use of these discoveries, medical professionals may in the future be able to study a patient’s digestive tract bacteria to differentiate between DLB and Parkinson’s disease.
Importantly, the reduced levels of Bifidobacterium mayalsosuggest possible ways to treat DLB. A crucial protein that promotes the growth, development, and maintenance of neurons in the central and peripheral nervous systems, brain-derived neurotrophic factor, is increased by bifidobacterium. Therefore, its decrease in DLB is likely to be associated with cognitive decline.
Similar to Collinsella, Ruminococcus torques is an intestinal bacterium that carries an enzyme that controls inflammation in the substantia nigra, a part of the brain. Dopamine, a neurotransmitter important in the control of movement and inadequate in Parkinson’s disease, is produced by the substantia nigra.
These bacteria were present at higher levels in DLB patients compared to those with Parkinson’s disease. This could help to explain why DLB differs from Parkinson’s disease in that its effects on movement are delayed.
“Our findings can be used both for both diagnosis and treatment,” explains Ohno. “If a patient with Parkinson’s disease develops dementia in one year after the onset of motor symptoms, they are diagnosed with DLB. However, we cannot currently predict whether a patient with Parkinson’s disease will become a DLB patient. The gut microbiome will help to identify such patients.”
“In terms of treatment, the administration of Ruminococcus torques and Collinsella in patients with Parkinson’s is expected to delay neuroinflammation in the substantia nigra,” Ohno added. “Therapeutic intervention to increase Bifidobacterium may delay the onset and progression of DLB and reduce cognitive dysfunction.”
“The presence of intestinal bacteria unique to DLB may explain why some patients develop Parkinson’s disease and others develop DLB first,” Ohno said. “Normalizing the abnormal bacteria shared between DLB and Parkinson’s disease may delay the development of both diseases. Improving the gut microbiota is a stepping stone in the treatment of dementia. Our findings may pave the way for the discovery of new and completely different therapeutics.”