Prostate cancer cells, in theory, can spread anywhere in the body. In practice, however, prostate cancer metastasis most commonly occurs in the lymph nodes and bones. Prostate cancer metastasis occurs when cells in the prostate break away from the tumor. Cancer cells can spread to other parts of the body via the lymphatic system or the bloodstream.
If prostate cancer is discovered as a result of screening, it is likely to be at an earlier and more treatable stage than if no screening was performed. While this may appear to imply that prostate cancer screening is always beneficial, there are still issues surrounding screening that make it unclear whether the benefits outweigh the risks for most men.
The majority of prostate cancers remain localized, giving affected individuals a good chance of survival. However, approximately 20% of patients develop incurable metastatic prostate cancer, resulting in 5,000 deaths in Austria alone each year. Medical research has yet to explain why metastases occur in some people but not others. A MedUni Vienna research team has discovered specific changes in a protein that drive the growth and spread of prostate cancer. The findings were published recently in the journal Molecular Cancer.
Our study provides new insights into the previously poorly understood transition from localised prostate cancer to terminal metastatic prostate cancer.
Lukas Kenner
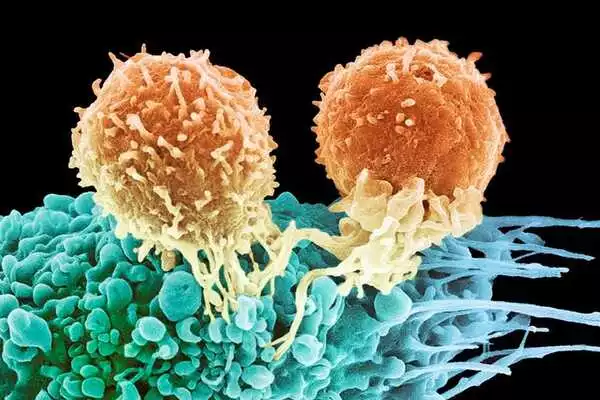
The researchers broke new ground in the study by looking into the role of the protein KMT2C in prostate cancer. KMT2C is a genetic component that primarily acts as a regulator of central cellular processes. If KMT2C loses this regulatory ability due to typical cancer-related mutations, this promotes the proliferation of the cancer gene MYC. This, in turn, causes cells to divide at a faster rate, causing the cancer to grow and spread.
Testing for prostate-specific antigen (PSA) levels in a man’s blood can often detect prostate cancer early. The digital rectal exam is another method of detecting prostate cancer (DRE). During a DRE, the doctor inserts a gloved, lubricated finger into the rectum to feel the prostate gland. These tests and the actual process of screening are described in more detail in Screening Tests for Prostate Cancer.
New insights into the transition to metastasis
“Our study provides new insights into the previously poorly understood transition from localized prostate cancer to terminal metastatic prostate cancer,” says study leader Lukas Kenner (Department of Pathology at MedUni Vienna, Comprehensive Cancer Center of MedUni Vienna and University Hospital Vienna, Department of Laboratory Animal Pathology at Vetmeduni Vienna and the K1 Center CBmed), underlining the significance of the research work. In addition, the knowledge gained about the effects of KMT2C mutations may also generate new momentum for the diagnosis and treatment of prostate cancer.
Diagnosing aggressive progression at an early stage
A blood test can detect KMT2C mutations, allowing for early detection of potentially aggressive progression in prostate cancers. Furthermore, MYC inhibitors may be used to prevent increased cell division and thus metastasis, and it is hoped that further scientific research will support this. MYC inhibitors are essentially new cancer treatment drugs that have already been tested in clinical trials and could be used in metastatic prostate cancer in the coming years if further studies confirm this.
“Because a high level of KMT2C mutation characterizes many types of cancer, including breast, lung, colorectal, bladder, and even skin cancer,” says Lukas Kenner, “our study results have a great deal of potential in the research, diagnosis, and treatment of malignant cancers in general.”