As the environment changes, temperature isn’t the sole element influencing the spread of infectious diseases. Humidity also plays a role, according to new research published this week (February 25) in Ecology Letters. The international team, led by Penn State researchers, created a model to investigate how parasitic worms, specifically species that infect livestock and wildlife, respond to temperature and humidity changes, and how these variables may shape the risk of infection and the formation of new hot spots in the future. The findings, which may indicate comparable behavior in worms that infect humans, could inform cattle management and public health measures in endemic areas.
“We need to understand how climate change can affect the future of these infections,” said Isabella Cattadori, a Penn State biology professor and the study’s principal author. “Will they get worse? Will they go into various environments and establish new hotspots? Will they mutate and become more pathogenic infections?”
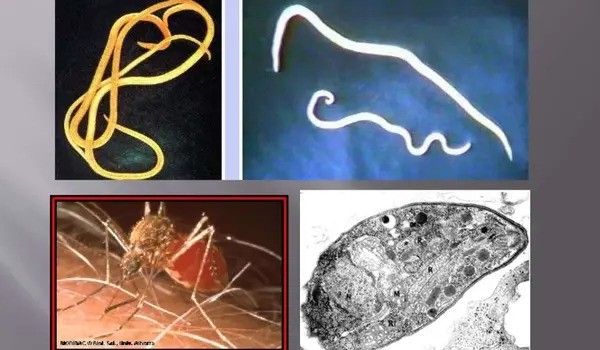
According to the World Health Organization, parasitic worms, notably soil-transmitted helminths, are widespread, infecting around 25% of the world’s population. They are also a major source of infection in animals, resulting in significant economic loss for the livestock industry. However, Cattadori stated that studies on the environment and illnesses often focus on diseases transmitted by vectors such as mosquitoes and ticks.
We need to understand how climate change can affect the future of these infections. Will they get worse? Will they go into various environments and establish new hotspots? Will they mutate and become more pathogenic infections?
Isabella Cattadori
“There isn’t much attention on helminth infections because they’re not as threatening as vector-borne diseases, and people tend to underestimate the importance of worm infections,” Cattadori said, further explaining that most studies focus on temperature, and few consider other climate-related variables, like humidity, as drivers of infection.
The lifecycle of soil-transmitted helminths has two phases — a free-living stage as eggs and larvae in the environment and an adult stage inside the host. Researchers sought to understand how the free-living stages were affected by climate. They reviewed current scientific literature to gather data on the effect of temperature and relative humidity on helminth egg and larval stages of nine species of helminth that commonly infect livestock and wildlife. These species were then divided into two groups depending on where they reside in their host: worms that live in the stomach and worms that live in the intestines.
Based on this information, they developed a mathematical model to describe how helminth hatching, development, and mortality of each helminth group responds to temperature and humidity. They then applied this model to look at historical and future projections of infection risk under different climate change scenarios across Southern, Central, and Northern Europe. For future projections, they considered short-term, from 2041 to 2060, and long-term, from 2081 to 2100, scenarios.
“We didn’t just look at correlation or linear relationships between variables. We disentangled how each component of the free-living stages is affected by climatic conditions, developing a mechanistic understanding of how helminths respond to these environmental stressors,” said Chiara Vanalli, a postdoctoral scholar at Penn State and lead author of the study, which she conducted as a graduate student in Cattadori’s lab. “This is essential for understanding what might happen in the future.”
The study is one of the first, Cattadori said, to look at the interaction between multiple climate variables across multiple parasitic worm species to understand how these factors may alter the seasonal profile of disease transmission, as well as when and where these patterns might arise.
Researchers discovered that not all parasite species behave the same way. Those that reside in the host’s intestines were strongly affected by temperature, reaching the highest risk of infection at 50 degrees Fahrenheit. On the other hand, helminths that reside in the stomach responded strongly to humidity, reaching their peak when humidity was 80% or higher. When researchers looked at the seasonality in these patterns across Europe, they found that historically, infection risk has one or two peaks in the spring and summer for the intestinal group and one peak for the stomach group. However, in the future, they expect these peaks may change.
“The intensity of these peaks and the way they shift will depend on location and specific climatic conditions as well as helminth species type,” Vanalli said. A two-season trend, with one peak in spring and one in fall, is expected to intensify for intestinal helminths while stomach helminths may be more likely to maintain the summer peak, especially at northern regions.
Researchers also evaluated how the spatial distribution might alter. Historically, infection risk has been low in Northern Europe. However, when researchers looked into the future, they discovered that infection hotspots will relocate north, aided by growing milder climates in central and northern regions, while southern regions will experience more harsh temperatures and droughts. Over time, Scandinavian countries are expected to face the highest danger from both types of helminths, with an increase of up to 100% for intestinal species and 55% for stomach species compared to the rest of the continent. Furthermore, the dramatic rise in infection risk at mid-to-high latitudes may exacerbate the chance of co-infection, as different helminth species can coexist.
With a better understanding of how animals are exposed to these infections and potential changes in the future, the findings could lead to the development of better livestock management and preventative control strategies, the researchers said. The dynamics described by the researchers could also shed light on the potential risk for human health because some of the family groups studied include parasites that also affect humans.
















