A new study has discovered a new biomarker that indicates resilience to chronic stress. This biomarker is largely absent in people suffering from major depressive disorder, and its absence is linked to pessimism in daily life, according to the study. Emory University scientists published their findings in Nature Communications.
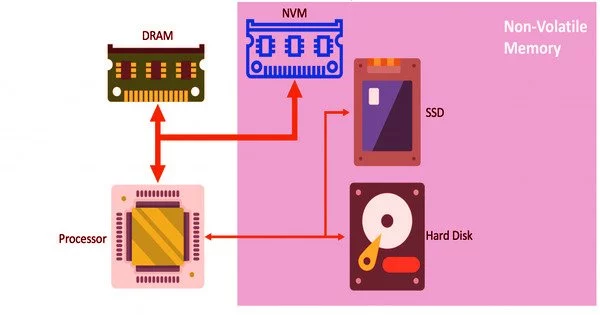
The researchers used brain imaging to look for differences in the neurotransmitter glutamate in the medial prefrontal cortex before and after the study participants completed stressful tasks. They then followed the participants for four weeks, using a survey protocol to assess how they rated their expected and experienced outcomes for daily activities on a regular basis.
“To the best of our knowledge, this is the first study to show that glutamate in the human medial prefrontal cortex exhibits adaptive habituation to a new stressful experience if someone has recently experienced a lot of stress,” says Michael Treadway, senior author of the study and professor in Emory’s Departments of Psychology and Psychiatry and Behavioral Science.
“Importantly, this habituation is significantly altered in depressed patients. We believe this is one of the first biological signals of its kind to be discovered in relation to stress and clinical depression.”
A new study identifies a novel biomarker indicating resilience to chronic stress. This biomarker is largely absent in people suffering from major depressive disorder, and this absence is further associated with pessimism in daily life, the study finds.
“Learning more about how acute and chronic stress affect the brain may aid in the identification of treatment targets for depression,” says Jessica Cooper, the study’s first author and a postdoctoral fellow in Treadway’s Translational Research in Affective Disorders Laboratory. The lab’s research focuses on the molecular and circuit-level mechanisms underlying psychiatric symptoms such as mood disorders, anxiety, and decision-making.
Stress has long been recognized as a major risk factor for depression, one of the most common and debilitating mental illnesses. “Depression is, in many ways, a stress-related disorder,” Treadway says. “It is estimated that significant, chronic life stress precedes 80 percent of first-time depressive episodes.”
Approximately 16 to 20% of the U.S. population will meet the criteria for a major depressive disorder at some point in their lives. Experts predict that depression rates will rise even further as a result of the ongoing COVID-19 pandemic. According to the Kaiser Family Foundation, approximately four in ten adults in the United States have reported symptoms of anxiety or depressive disorder during the pandemic, up from one in ten in 2019.
“The pandemic has increased many people’s isolation while also increasing the number of severe stressors and existential threats they face,” Treadway says. “That combination puts a lot of people at a high risk of depression.”
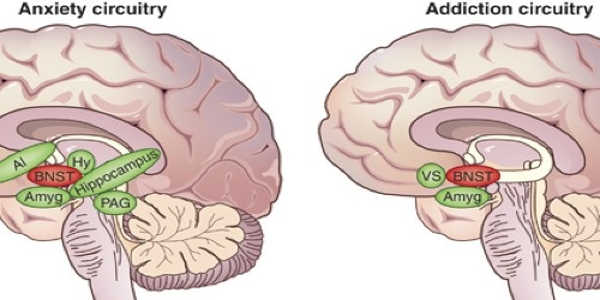
Although the link between stress and depression is well established, the mechanisms underlying this relationship are not well understood. Experiments with rodents have revealed a link between stress and the response of glutamate, the major excitatory neurotransmitter in the mammalian brain. The role of glutamate in humans suffering from depression, on the other hand, has been less clear.
The current study included 88 people who did not have a mental health disorder and 88 unmedicated patients who were diagnosed with a major depressive disorder. Before being subjected to experiments involving a brain scanning technique known as magnetic resonance spectroscopy, participants were polled about their perceptions of recent stress in their lives.
While in the scanner, participants were required to alternate between two tasks that served as acute stressors: placing their hand up to their wrist in ice water and counting down from the number 2,043 by 17 steps while someone evaluated their accuracy.
Before and after the acute stressor, brain scans measured glutamate in the medial prefrontal cortex, an area of the brain involved in thinking about one’s state and forming expectations. Previous research has also revealed that this brain region is involved in the regulation of adaptive responses to stress.
While in the scanner, participants provided saliva samples, which allowed the researchers to confirm that the tasks elicited a stress response by measuring the amount of the stress hormone cortisol in the sample.
Brain scans in healthy people revealed that individual levels of recent perceived stress predicted glutamate change in response to stress in the medial prefrontal cortex. Healthy participants with lower levels of stress had higher glutamate levels in response to acute stress, whereas healthy participants with higher levels of stress had lower glutamate levels in response to acute stress. This adaptive response was notably lacking in patients suffering from depression.
“The decrease in glutamate response over time appears to be a signal, or marker, of a healthy adaptation to stress,” says Treadway. “And if the levels remain high, it appears to be a sign of maladaptive stress responses.”
The initial result for adaptation in healthy participants was strong, but it was in small sample size, so the researchers decided to see if they could replicate it. Treadway says, “Not only did we get a replication, but it was an unusually strong replication.”
A group of healthy controls was also included in the experiment, and they were scanned before and after performing tasks. Rather than stressful tasks, the controls were instructed to place their hands in warm water or to count out loud consecutively. Their glutamate levels were not related to their perception of stress, and they did not exhibit a salivary cortisol response.
The researchers followed participants for four weeks after scanning to broaden their findings. Every other day, the participants reported on their expected and actual outcomes for daily activities. The findings revealed that glutamate changes that were higher than expected based on an individual’s perceived stress level predicted an increased pessimistic outlook – a hallmark of depression.
Cooper explains, “We were able to show how a neural response to stress is meaningfully related to what people experience in their daily lives.” “We now have a large, rich data set to build on as we continue to investigate how stress contributes to depression.” The National Institutes of Mental Health funded the research.