Spending too much time in the sun is the main cause of skin cancer. Sunlight has ultraviolet (UV) rays that can change the DNA in skin cells in ways that lead to cancer. Sunlamps, tanning booths, and X-rays also make these UV rays that damage skin. It can usually be cured, but the disease is a major health concern because it affects so many people. About half of fair-skinned people who live to age 65 will have at least one skin cancer. Most can be prevented by protecting your skin from the sun and ultraviolet rays.
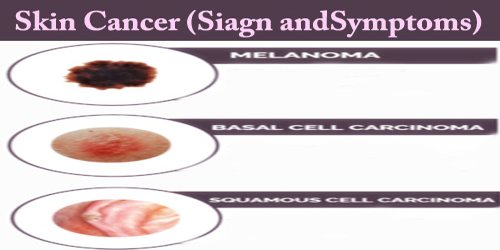
The main types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma, which originates from the pigment-producing skin cells (melanocytes) but is less common, though more dangerous, than the first two varieties. Other rare forms of skin cancer include lymphomas, Merkel cell cancers, and cancers of other tissue in the skin, including sarcomas as well as hair and sweat gland tumors.
Sign and Symptoms –
Since most skin cancers are caused by ultraviolet light exposure, skin cancers are generally not considered to be inherited. But the fact that skin cancer is much more common among poorly pigmented individuals and that skin color is inherited does support the proposition that genetics are very important. There are some very rare genetic syndromes that result in an increased number of skin cancers in those affected.
The general warning signs of skin cancer include:
- Any change in size, color, shape, or texture of a mole or other skin growth
- An open or inflamed skin wound that won’t heal
Melanoma, the most dangerous type of skin cancer, may appear as:
- A change in an existing mole
- A small, dark, multicolored spot with irregular borders either elevated or flat that may bleed and form a scab
- A cluster of shiny, firm, dark bumps
- A mole larger than a pencil eraser
Basal cell carcinoma usually occurs in sun-exposed areas of our body, such as our neck or face.
Basal cell carcinoma may appear as:
- A pearly or waxy bump
- A flat, flesh-colored or brown scar-like lesion
- A bleeding or scabbing sore that heals and returns
Most often, squamous cell carcinoma occurs on sun-exposed areas of our body, such as our face, ears, and hands. People with darker skin are more likely to develop squamous cell carcinoma on areas that aren’t often exposed to the sun.
Squamous cell carcinoma may appear as:
- A firm, red nodule
- A flat lesion with a scaly, crusted surface
Other, less common types of skin cancer include:
- Kaposi sarcoma. This rare form of skin cancer develops in the skin’s blood vessels and causes red or purple patches on the skin or mucous membranes. Kaposi sarcoma mainly occurs in people with weakened immune systems, such as people with AIDS, and in people taking medications that suppress their natural immunity, such as people who’ve undergone organ transplants. Other people with an increased risk of Kaposi sarcoma include young men living in Africa or older men of Italian or Eastern European Jewish heritage.
- Merkel cell carcinoma. Merkel cell carcinoma causes firm, shiny nodules that occur on or just beneath the skin and in hair follicles. Merkel cell carcinoma is most often found on the head, neck and trunk.
- Sebaceous gland carcinoma. This uncommon and aggressive cancer originates in the oil glands in the skin. Sebaceous gland carcinomas which usually appear as hard, painless nodules can develop anywhere, but most occur on the eyelid, where they’re frequently mistaken for other eyelid problems.
Actinic keratoses (AK), also called solar keratoses, are scaly, crusty lesions caused by damage from ultraviolet light, often in the facial area, scalp, and backs of the hands. These are considered precancers because if untreated, up to 10% of actinic keratoses may develop into squamous cell carcinomas.
Diagnosis –
The world’s most common cancer is a relentless disease that strikes one in five people by age 70. The good news is that 99 percent of all cases are curable if they are diagnosed and treated early enough. But in order to stop skin cancer, we have to spot it on time. Unlike cancers that develop inside the body, skin cancers form on the outside and are usually visible. That’s why skin exams, both at home and with a dermatologist, are especially vital.

To diagnose skin cancer, a patient’s doctor may:
- Examine the patient’s skin. The doctor may look at their skin to determine whether their skin changes are likely to be skin cancer. Further testing may be needed to confirm that diagnosis.
- Remove a sample of suspicious skin for testing (skin biopsy). The doctor may remove the suspicious-looking skin for lab testing. A biopsy can determine whether any people have skin cancer and, if so, what type of skin cancer they have.
- Skin growths that are most likely basal cell carcinoma, squamous cell carcinoma, or other forms of non-melanoma can be biopsied in various ways. Part or all of the growth can be taken with a scalpel for examination under a microscope.
Additional tests might include imaging tests to examine the nearby lymph nodes for signs of cancer or a procedure to remove a nearby lymph node and test it for signs of cancer (sentinel lymph node biopsy). Doctors use the Roman numerals I through IV to indicate cancer’s stage. Stage I cancers are small and limited to the area where they began. Stage IV indicates advanced cancer that has spread to other areas of the body.
Treatment –
Most skin cancers are detected and cured before they spread. Standard treatments for localized basal cell and squamous cell carcinomas are safe and effective and cause few side effects. Small tumors can be surgically excised, removed with a skin scraping and electric current cauterization, frozen with liquid nitrogen, or killed with low-dose radiation. Melanoma that has spread to other organs presents the greatest treatment challenge.
There are several effective means of treating skin cancer. The choice of therapy depends on the location and size of the tumor, the microscopic characteristics of cancer, and the general health of the patient.
- Topical medications: In the case of superficial basal cell carcinomas, some creams, gels, and solutions can be used, including imiquimod (Aldara), which works by stimulating the body’s immune system causing it to produce interferon which attacks cancer, and fluorouracil (5-FU), a chemotherapy drug. Some patients do not experience any side effects of these topical treatments, but others may have redness, inflammation, and irritation. A drawback of topical medications is that there is no tissue available to examine to determine if a tumor is removed completely.
- Destruction by electrodesiccation and curettage (EDC): The tumor area is numbed with a local anesthetic and is repeatedly scraped with a sharp instrument (curette), and the edge is then cauterized with an electric needle. The advantage of this method is that it is fast, easy, and relatively inexpensive. The disadvantages are that the scar is often somewhat unsightly, and the recurrence rate is as high as 15%.
- Surgical excision: The area around the tumor is numbed with a local anesthetic. A football-shaped portion of tissue including the tumor is then removed and then the wound edges are closed with sutures. For very big tumors, skin grafts or flaps are needed to close the defect. The advantages of this form of treatment are that there is a greater than 90% cure rate, the surgical specimen can be examined to be sure that the whole tumor is successfully removed, and the scar produced is usually more cosmetically acceptable than that of the EDC procedure. It is a more complicated procedure and is more expensive than EDC.
- Mohs micrographic surgery: The site is locally anesthetized and the surgeon removes the visible tumor with a small margin of normal tissue. The tissue is immediately evaluated under a microscope and areas that demonstrate residual microscopic tumor involvement are re-excised and the margins are re-examined. This cycle continues until no further tumor is seen. This more complicated and expensive option is the treatment of choice for tumors where normal tissue preservation is vital, where the tumor margins are poorly defined, in tumors that have been previously treated and have recurred, and in certain high-risk tumors.
- Radiation therapy: Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation therapy may be an option when cancer can’t be completely removed during surgery. This form of treatment is useful in those who are not candidates for any surgical procedure. The advantage of radiation therapy is that there is no cutting involved. The disadvantages of this expensive alternative are that the treated area cannot be tested to be sure the whole tumor is gone and radiation scars look worse over time. It is for this reason it is usually reserved for elderly patients.
- Photodynamic and Biological therapy: Photodynamic treatment destroys skin cancer cells with a combination of laser light and drugs that makes cancer cells sensitive to light. Biological therapy uses your body’s immune system to kill cancer cells.
Retinoic acid may inhibit cancer recurrence in patients who have had tumors removed, but there is a lack of evidence to support either of these treatments. Other types of treatments for skin cancers include cryosurgery where tissue is destroyed by freezing, photodynamic therapy (PDT) in which medication and blue light is used to destroy the cancerous tissue, laser surgery to vaporize (ablate) the skin’s top layer and destroy lesions, and oral medications vismodegib (Erivedge) and sonidegib (Odomzo).
The prognosis for nonmelanoma skin cancer is generally excellent. Both basal cell carcinoma and squamous cell carcinoma are highly curable. There are virtually no deaths from basal cell carcinoma and only rare deaths with squamous cell carcinoma skin cancers, mostly in immunosuppressed individuals. Depending on the method of treatment and the location and type of skin cancer, the likelihood of a recurrence of a previously treated skin cancer is as low as 1% to 2% for Mohs surgery and up to 10% to 15% for destruction by electrodessication and curettage.
Early detection of skin cancers can lead to better outcomes. Know our skin and if we have any moles or spots that are suspect, see a dermatologist for a skin cancer screening. Awareness is key in identifying and treating skin cancers early.
Information Sources: