Accelerating a process that slows with age may protect against atherosclerosis, a significant cause of heart attacks and strokes. Scientists have successfully reduced the development of artery-narrowing plaque in mice that would otherwise develop the lesions. The researchers achieved this by increasing chaperone-mediated autophagy (CMA), a cellular cleaning mechanism.
Scientists at Albert Einstein College of Medicine, lead by Ana Maria Cuervo, M.D., Ph.D., successfully reduced artery-narrowing plaque in mice that would otherwise develop those lesions, according to data published online today in Proceedings of the National Academy of Sciences (PNAS). The researchers achieved this by increasing chaperone-mediated autophagy (CMA), a cellular housekeeping mechanism identified by Dr. Cuervo in 1993 and termed in 2000.
“We’ve shown in this research that we need CMA to protect against atherosclerosis, which becomes severe and progresses when CMA declines – something that also happens as people age,” said Dr. Cuervo, a professor of developmental and molecular biology and medicine, the Robert and Renée Belfer Chair for the Study of Neurodegenerative Diseases, and co-director of Einstein’s Institute for Aging Research. “But, more importantly, we’ve shown that raising CMA activity can be a successful method for slowing and stopping the progression of atherosclerosis.”
An Impressive CMA CV
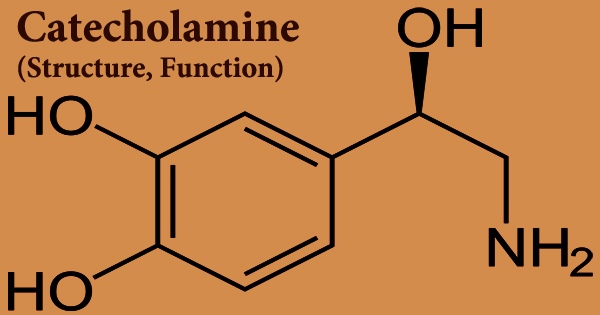
CMA maintains normal cell function by selectively destroying the numerous proteins found in cells. In CMA, specific “chaperone” proteins link to proteins in the cytoplasm and direct them to enzyme-filled cellular compartments known as lysosomes, where they are digested and recycled. Dr. Cuervo has identified many of the molecular actors involved in CMA and demonstrated that CMA regulates multiple intracellular processes including as glucose and lipid metabolism, circadian rhythms, and DNA repair through the timely degradation of critical proteins. She also discovered that disturbed CMA allows damaged proteins to accumulate to toxic levels, which contributes to aging and neurodegenerative illnesses such as Parkinson’s, Alzheimer’s, and Huntington’s disease when the toxic buildup occurs in nerve cells.
We’ve shown in this research that we need CMA to protect against atherosclerosis, which becomes severe and progresses when CMA declines – something that also happens as people age. But, more importantly, we’ve shown that raising CMA activity can be a successful method for slowing and stopping the progression of atherosclerosis.
Professor Dr. Cuervo
Dr. Cuervo’s accomplishments were recognized when she was elected to the National Academy of Sciences in 2019. (NAS). In 1996, the NAS started encouraging newly elected members to submit a special Inaugural Article to PNAS that highlighted the member’s scientific contributions. Due to COVID-19 pandemic-related delays, Dr. Cuervo’s research on CMA’s preventive effect against atherosclerosis is her first PNAS paper, and it adds to her corpus of work on the relevance of CMA.
Fighting Back Against Plaque
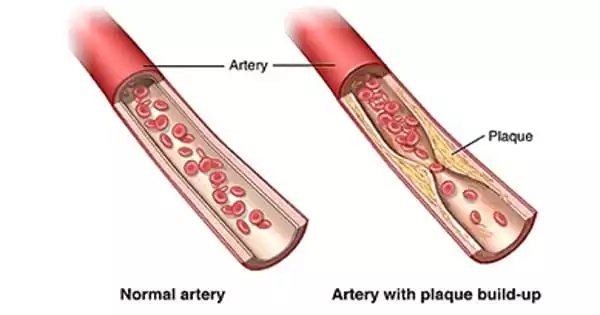
Cardiovascular disease (CVD) is the leading cause of death worldwide, with heart attacks and strokes accounting for more than 80% of CVD deaths. CVD is typically associated with atherosclerosis, which is the accumulation of plaque (a sticky mass composed of fat, cholesterol, calcium, and other substances) within the artery walls. Plaque hardens and narrows arteries, preventing oxygenated blood from reaching the heart muscle (leading to heart attacks), the brain (strokes), and the rest of the body.
Dr. Cuervo and colleagues investigated CMA’s role in atherosclerosis in mice by feeding them a fatty Western diet for 12 weeks and measuring CMA activity in the animals’ plaque-affected aortas. CMA activity increased initially in response to the dietary challenge; however, plaque buildup was significant after 12 weeks, and virtually no CMA activity could be detected in the two types of cells known to malfunction in atherosclerosis, leading to the buildup of plaque within arteries — macrophages and arterial smooth muscle cells.
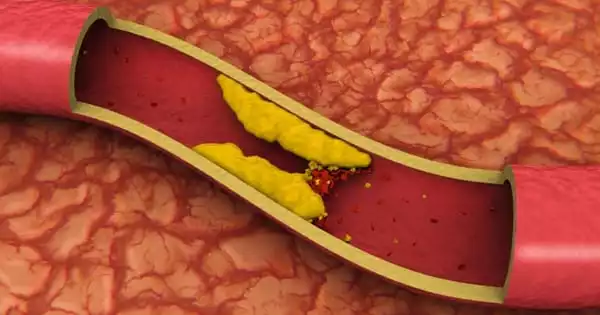
“CMA seemed to be very important in protecting macrophages and smooth muscle cells — helping them function normally despite the pro-atherosclerotic diet — at least for a while, until their CMA activity basically came to a halt,” said Dr. Cuervo. She noted that feeding the high-fat diet to mice totally lacking in CMA activity produced even stronger evidence of CMA’s importance: plaques nearly 40% larger than those in control animals that were also on the high-fat diet.
Of Mice and Also Men Fig: Researchers find new strategy for preventing clogged arteries
The researchers discovered evidence that low CMA activity associated with atherosclerosis in humans as well. To lessen the risk of a second stroke, some stroke victims undergo a surgical treatment known as carotid endarterectomy, which eliminates plaque-affected parts of their carotid arteries. Dr. Cuervo and colleagues looked examined CMA activity in carotid artery segments from 62 first-time stroke patients who were followed for three years following surgery.
“Those patients with higher levels of CMA following their first strokes never got a second one, while second strokes occurred in nearly all the patients with low CMA activity,” said Dr. Cuervo. “This suggests that your CMA activity level post-endarterectomy could help in predicting your risk for a second stroke and in guiding treatment, especially for people with low CMA.”
Turning Up CMA, Tuning Out Atherosclerosis
The study is the first to indicate that increasing CMA levels may be an effective method to prevent atherosclerosis from worsening or advancing. The researchers genetically “upregulated” CMA in mice fed a pro-atherosclerotic, high-fat Western diet for 12 weeks before comparing them to control animals fed the same diet. When compared to the control mice, the CMA-boosted mice had significantly improved blood lipid profiles, with much lower levels of cholesterol. Plaque lesions developed in genetically engineered mice were substantially smaller and less severe than plaques in control mice. Fortunately, no genetic changes are required for people to profit from this discovery.