INTRODUCTION:
In Bangladesh the incidence of Chronic Suppurative Otitis Media (CSOM) is very high because of poor socio-economic condition, over crowding, poor nutrition and lack of health-education (Amin et al., 1989).
Among the two types of chronic suppurative otitis media (tubotympanic and attico-antral variety) tubotympanic variety is the commonest and is called safe as the risk of complications are less (Ludman, 1998). The name, tubotympanic, indicates disease which is limited to the Eustachian tube and tympanic cavity and is always characterized by perforation in the tympanic membrane. The perforation is always central involving the pars tensa, of varying size and shape with remnants of tympanic membrane and is usually with part or all of the manubrium of the malleus remaining. The perforation of the tympanic membrane is usually associated with aural discharge and hearing loss. Discharge is usually mucoid or mucopurulent but becoming purulent and profuse during exacerbations. It is usually intermittent and recurring whenever there is upper respiratory tract infection or if water enters into ear accidentally.
Hearing loss occurring from chronic suppurative otitis media is a burden to the individual and also to the family and entire society. The predominant hearing loss in tubotympanic disease is conductive in nature. A perforation in the tympanic membrane reduces the effective area of membrane in contact with the sound wave. Perforations also reduce the pressure differential across the tympanic membrane and depending on their position, reduce the mechanical coupling between the remaining intact portions of the membrane and the malleus (Kerr, 1997).
There is a significant quantitative correlation between the size and site of perforation and hearing loss. Small perforations (10% of the membrane) produce losses of 10-15 dB below 3 KHz. Large perforations produce severe losses over the whole range particularly at higher frequencies, through these perforations, the sound waves act directly on the round & oval windows. Small and moderate perforations (10-40% of the area) have far more severe effects when placed on the posterior and superior part of the membrane than when placed on the anterior and inferior parts (Kerr, 1997). However, non-marginal perforation with intact ossicular chain hearing loss is approximately 10-30 dB (Yung, 1995)
Myringoplasty is the operation specifically designed to repair or reconstruct the tympanic membrane. The earliest reported successful myringoplasty was done by Berthold in 1878, using full thickness skin graft. Since then, myringoplasty has gone through many changes in techniques and materials. Shea in 1960 first introduced underlay technique for myringoplasty and used vein as graft material. Autologus temporalis fascia was used as graft material firstly by Heerman in 1960.
A successful myringoplasty controls recurrent infection, improves hearing, prevents tympanosclerosis & cochlear degeneration and hearing-aid use. Myringoplasty has been suggested to protect the middle ear by preventing the progression of ossicular pathology and preventing cholesteatoma formation (Ludman, 1998).
The prerequisites of myringoplasty are dry central perforation of tympanic membrane in CSOM, free of any pathological lesion in the external ear, middle ear and mastoid, functioning eustachian tube and no systemic diseases like
diabetes mellitus, hypertension etc.
The surgical outcome of myringoplasty is influenced by many factors. The reported success rate of myringoplasty is therefore variable, partly because of differences in the inclusion and exclusion criteria. In Bhatt’s (2000) study, the overall success rate of myringoplasty was 86%, where posterior & inferior perforations had 90% success rate after repair, compared to only 67% in anterior perforations. This was due to poor access to anterior perforations. There is a linear relationship between the size of perforation and success of operation, smaller perforations having better success rates than larges ones (Sade et al., 1981) Vrabec et al. (1997) found poorer results in younger patients and better success with advancing age. This is due to lower incidence of upper airway infections and better eustachian tube function in advancing age and the relative immaturity of the immune system in younger children. Caylon et al. (1998) found no statistical difference in the success rate between two sex groups. Lorenzo et al. (2001) found better success rate in underlay than overlay technique. The success rate was 82.3% in the underlay and 79.1% in the overlay technique (Lorenzo et al., 2001).
At present, Myringoplasty is a common operation in the otolaryngology department, having microsurgical facilities. The present study aims at evaluating the surgical results of myringoplasty in selected patients with tympanic membrane perforation and assessing the factors potentially influencing there outcome. For this purpose, the following hypothesis has been proposed:
Hypothesis:
Myringoplasty is a useful procedure for preservation and improvement of hearing in Chronic Suppurative Otitis Media of tubo-tympapnic variety.
RATIONALITY OF THE STUDY:
In Bangladesh, CSOM is a very common condition. Conventionally conservative treatment is usually given to control the infection but if the infection is not adequately controlled, then surgical intervention, such as myringoplasty is done to prevent infection and improve hearing status of the affected person. The present work has been undertaken to perform myringoplasty in the above mentioned condition
AIMS AND OBJECTIVES
A. General –
(i) To assess the graft-take rate after myringoplasty.
(ii) To assess the hearing status after myringoplasty.
B. Specific –
To compare the graft-take rate with regard to –
(i) Age of the patients
(ii) Sex of the patients
(iii) Site of the perforations
(iv) Size of the perforations
(v) Approach of the surgery
REVIEW OF LITERATURE
RELATED PREVIOUS STUDY
Bhuiyan (2003) carried out a study in 2003 at the department of Otolaryngology and Head-Neck surgery, BSMMU and DhakaMedicalCollegeHospital, Dhaka with the aim to establish ways of improving results in myringoplasty. The study included 50-myringoplasty operations. The overall success rate was 84%. Of the successful cases hearing was improved in 27 patients (64.28%) and 15 patients (35.71%) of the successful cases showed no significant improvement of hearing.
Another study on myringoplasty was carried out by Ekramuddoula (2002), at the department of Otolaryngology and Head-Neck Surgery of Dhaka Medical College Hospital, Dhaka with the aim to assess the graft-take rate as well as hearing improvement. This study included 50 patients those underwent myringoplasty operation with temporalis fascia graft. In this study graft-take rate was 80% and graft failure was 20%. Of the successful cases hearing was improved in 24 patients (60%) and 16 patients (40%) of successful cases had no hearing improvement.
Results of myringoplasty operation presenting various techniques have already been reported by numerous surgeons (Austin, and Shea, 1961, Guilford, 1962, Jansen, 1964, Cody and Taylor 1973, Glasscock 1973, Puhakka et al., 1979).
Derlacki (1953) carried out a study on 131 patients having dry central perforation of which 99 (75.6%) cases were successful closure and 32 cases (24.4%) were failure. Nine cases of successful closure had perforation, occurring within two months to one year. Ninety nine patients (successful cases) showed an average hearing gain of 16.3 dB. Seven patients had no gain of hearing (Derlacki, 1953).
Cody and Taylor (1973) repaired 878 tympanic membrane perforations by different graft materials (canal skin and fascia, single fascia, double fascia, canal skin and homograft tympanic membrane). The percentage of successful graft was 82%. Of the 878 tympanoplasties, 157 (18%) failed. Of all 878 operations, 129 (15%) failed early and 13 (1.48%) failed after six months and 15 failed after 18 months. Only 79% of the operation achieved a socially adequate hearing level. The air-bone gap was closed to with 15dB (Cody and Taylor, 1973).
Doyle et al. (1972) conducted one of the few studies comparing overlay and underlay techniques of tympanoplasty. The overlay technique was used in 52 cases and the underlay technique was used for 79 cases. All cases were done through endaural approach. The overall failure rate in overlay technique after one year and two years were 36%. Hearing was improved up to 15dB level in 27%, unchanged in 50% and worse in 23%. The overall failure rate in underlay techniques was 14%. Hearing was improved in 62%, unchanged in 31% and worse in 7%. Doyle et al. concluded that in experienced residents the medial grafting of the tympanic membrane gave better healing and fewer complication (Doyle et al., 1972).
Glasscock et al. (1972) carried out a study on 180 postauricular underlay cases. The underlay technique had a 96% graft-take rate. Of the failures, 4 were due to postoperative infection, one was a late perforation and two were due to technical error in graft placement (Glasscock et al., 1972).
Sade et al. (1981), during the year 1971-1979, carried out a study on 855 myringoplasty patients for short-term and long-term results. The operations were performed by experienced surgeon and by senior residents. Senior residents had very favourable results (success rate was 93.5%). Success rate of experienced surgeon was 63.5%. The initial graft-take rate was 81%. Follow-up after 1 year or more of successful cases showed that small perforation developed once again 8%, 8.7% showed tympanic membrane retraction, 11% showed some defect of the epithelial covering (Sade et al., 1981).
Ajmal et al. (2004) carried out a study on 60 patients of myringoplasty. In their study 20 patients had small central perforations, in 25 patient had medium size central perforations and large central perforation was present only in 15 patients. Success rate was 60%. Infection was the only complication, which led to failure of myringoplasties 24 patients (40%) (Ajmal et al., 2004)
Sheehy and Anderson (1990) reviewed 472 cases of overlay tempanoplasties. They have showed a graft-take rate of 97%, when fascia was used and a graft-take rate was 84%, when canal skin was used. Post operatively 80% had air-bone gap within 10dB, with 58% of cases with air-bon gap within 5dB (Sheehy and Anderson, 1990).
HISTORICAL BACKGROUND:
Myringoplasty is an operative procedure used in the reconstruction of a perforation of the tympanic membrane. This assumes that the middle ear cavity, it mucosa, and the ossicular chain are free of active infection.
The term myringoplasty was coined by Berthold in 1878 but the first myringoplasty was performed by Marcus Bancer in 1640. Berthold placed a court plaster against the tympanic membrane for three days to remove the epithelium and then applied a thick skin graft. Despite success reported in two cases, little more was heard of myringoplasty until Schultof and Vadez mentioned it in 1944, and then not again until 1952 when Wullstein published a method of closing perforation with a split thickness skin graft. These operations were designed to restore or conserve hearing and promote healing after the excision of disease from the middle ear and mastoid. Only a year later Zollner described his experience with a similar graft; Wullstein and House then advised a full thickness graft taken from behind the ear. In 1961 Storrs used temporal fascia in order to close a tympanic membrane perforation. Over the past three decades temporal fascia has been the most commonly used grafting materials in myringoplasty or tympanoplasty operation, although tragal perichondrium, periosteum, loose overlay tissue, fat, vein and homologus dura were also employed.
House and Shea and Glasscock developed techniques for creating a satisfactory onlay graft. Shea in 1960 accidentally tore the tympanic membrane during a stapedectomy procedure and repaired the tear successfully with a free autologus vein graft, placed medial to the tympanic membrane, thus introducing the underlay technique of myringoplasty. Storrs switched to fascia and Paterson et al. determined the reason for the success of fascia as a grafting material. The popularity and success of the techniques of myringoplasty or tympanoplasty can be attributed to the success of many other surgeons who have refined others techniques.
ANATOMY OF THE EAR:
Both anatomically and functionally, the ear is divided into three parts: the external ear, the middle ear, and the inner ear.
THE EXTERNAL EAR
The external ear is the portion of the ear external to the tympanic membrane. It consists of the auricle and passage leading to the tympanic membrane, the external auditory canal.
The external auditory meatus is a tortuous canal of about 24 mm in length and extends from floor of the concha to the tympanic membrane. Its lateral one-third is cartilaginous and medial two-third is bony.
THE MIDDLE EAR CLEFT
The middle ear cleft consists of the Eustachian tube, middle ear cavity, aditus ad antrum, mastoid antrum and mastoid air cell system. The tympanic membrane forms the boundary between the external auditory meatus and the middle ear cavity.
The tympanic membrane is a thin semi-transparent membrane set obliquely at the medial end of external auditory meatus. It is functionally a part of the tympanic cavity. When viewed under illumination, it presents a pearly-grey appearance with a triangular cone of reflected light, extending from the centre forwards and downwards. At the apex of the cone lies the most concave area known as the umbo. The handle of the malleus extends upwards from the umbo. In the upper part to the membrane the short process of malleus is seen. The anterior and posterior malleolar folds run anteriorly and posteriorly from the short process.
The anterior and posterior malleolar folds divide the membrane into a lower larger part, called pars tensa and an upper smaller part, called pars flaccida.
The middle ear cavity lies between tympanic membrane laterally and inner ear medially. It has the form of a biconcave disc and measures about 15 mm from above downward, 13 mm from before backwards. Its transverse diameter is very narrow, being about 2 mm at the narrowest part.
THE INNER EAR:
The inner ear lies in the petrous part of temporal bone and is called the labyrinth. It consists of a bony labyrinth and a membranous labyrinth. Between the membranous and bony labyrinth lies perilymph. The bony labyrinth is a series of cavities in the petrous part of the bone and has three parts: vestibule, cochlea and semicircular canals. The membranous labyrinth is a continuous series of communicating sacs and ducts within the bony labyrinth. It consists of utricle and saccule in the bony vestibule, membranous semicircular ducts in the bony semicircular canals and cochlear duct (Scala media) in the bony cochlea. The membranous labyrinth contains endolymph. The Reissner’s membrane separates the scale media from scala vestibuli, whereas the basilar membrane supports the organ of Corti and separates it from the scala tympani. Both scala vestibuli and scala tympani contain perilymph, which has a direct communication with cerebrospinal fluid
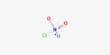
The Ear
A – The External Ear
1) The external auditory canal
2) The tympanic membrane
B – The Middle Ear
3) The hammer
4) The anvil
5) The stirrup
C – The Inner Ear
6) The semicircular canals
7) The cochlea
PHYSIOLOGY OF HEARING:
For physiological purposes, the ear is divided into two parts. The conducting apparatus consists of the external ear, tympanic membrane, chain of ossicles, eustachian tube and the labyrinthine fluids. The perceiving apparatus consists of the organ of Corti, auditory nerve and central connections.
CONDUCTION OF SOUND:
Most important route of sound transmission to the inner ear is through the ossicular chain. When sound waves from the external auditory canal meet the tympanic membrane, the membrane moves in and out. This causes malleus and incus to move in and out by rotating about an axis passing through the anterior ligament of malleus and short process of incus. The incus causes the stapes to rock around an axis passing vertically through the posterior border of the footplate. The movement of the footplate causes the cochlear fluids to set into vibration.
SENSORINEURAL MECHANISM OF HEARING:
Once the sound waves are transmitted along the middle ear, the movement of footplate of stapes causes the cochlear fluids to set into vibrations. The vibrations of subsonic frequency will produce a flow of perilymph up the scala vestibuli, through the helicotrema, and down the scala tympani to the round window membrane, which bulges outwards in opposite phase to the footplate. But with rapid vibrations of audiofrequencies, the acoustic impedance of the inner ear opposes this simple flow of perilymph and the acoustic energy causes a to and fro vibration of cochlear partitions. During this, the vibration of the basilar membrane results in a sliding or shearing movement between the tectorial membrane and the hair cells. The hairs of hair cells are thus displaced relative to their cell bodies and hair cells are stimulated due to this shearing force. As a result there is generation of cochlear microphonics and probably the final mechanical event preceding neuronal stimulation. Within cochlea the vibrations are processed and analyzed in such a way that the data representing frequency, intensity and phase relationships may be transmitted along the auditory nerve fibres to the brain.
PATHOLOGY
The chronic suppurative otitis media has been traditionally divided into two main types: tubotympanic and atticoantral.
Tubotympanic type the disease is usually confined within the mucosa with a central perforation in the pars tensa of the tympanic membrane and usually carries less risk to the patient of any serious complication. Hence it is called the safe type.
AETIOLOGY OF CHRONIC SUPPURATIVE OTITIS MEDIA
a) Environment: There is a close correlation between patients with chronic otitis media and socioeconomic groups; the lower groups having higher incidence. Possibly it relates to general health, diet and overcrowding in the home.
b) Infective: Bacterial infection of the mucosa is the main reason for continued activity of chronic suppurative otitis media. But it could be that bacteria are secondary invaders of mucosa, which was inflamed because of other factors, rather than they are the primary cause of the disease. However, wide range of microbes, both aerobic and anaerobic has been isolated from ears with chronic suppurative otitis media, including both gram-positive and gram-negative organisms. Most of the gram-positive organisms are Staph. aureus. But among the gram-negative organisms Pseud. aeruginosa, B. proteus, E.Coli and anaerobic bacteroides are the main offenders.
c) Upper respiratory tract infections: It is observed in most patients that their ears start to discharge after an upper respiratory tract infection. The mechanism may be that viral infection would also affect mucus of the middle ear making it less resistant to the organism normally present there, allowing bacterial overgrowth and subsequent active discharge.
d) Eustachian tubal dysfunction: Chronic dysfunction of the eustachian tube due to infection or anatomical obstruction in the nasopharynx may cause persistence of middle ear disease.
e) Previous otitis media: It appears to be generally held view that chronic suppurative otitis media is a sequelae of acute suppurative otitis media and/or secretory otitis media.
f) Genetic: Whether one race is more predisposed to chronic otitis media remains unanswered. It may be related to the size of the mastoid air cell system, which was once considered to be genetically determined.
g) Allergic: It is strongly believed that allergy is one of the causes of chronic suppurative otitis media
PATHOLOGY OF TUBOTYMPANIC DISEASE
Chronic suppurative otitis media is most often a recurrent rather than a constant disease and the pathological features encountered are characterized by lack of uniformity. In general, the following features are noted
The tympanic membrane: There is central perforation of the tympanic membrane and can be of any size and shape – sometimes large and reniform or situated non-marginally in the pars tensa.
The mucosa: The mucosa of the tympanic cavity is velvety and pink and may be oedematous. Occasionally a polypus, which is pedunculated and sometimes of considerable size, arises from inner tympanic wall. Rarely areas of ulceration and granulation tissue may occur.
Ossicles: The ossicles may or may not be damaged depending upon the severity of antecedent infection, commonly the long process of incus undergoes necrosis.
The mastoid: The mastoid is usually cellular but may be acellular. The mucosa of the mastoid air cells may show changes similar to those of the tympanic cavity and the cells may act as a reservoir of secretions
CLINICAL FEATURES OF CHRONIC SUPPURATIVE OTITIS MEDIA
Clinical feature of tubotympanic disease:
Discharge: The discharge is mucoid and intermittent but becomes purulent and foul smelling during exacerbation and in the presence of secondary invaders. It is profuse during upper respiratory tract infection.
Hearing loss: It is conductive in type. The degree varies with size and position of perforation, usually slight when it is small and anteriorly located.
Otoscopy: It shows perforation in the tympanic membrane, small, large or subtotal and non-marginally situated in the pars tensa. Polypoid change may be seen in the mucosa.
Clinical features of attico-antral disease
Malodorous otorrhoea – Ear discharge is usually scanty but has a peculiar offensive odour. It is sometimes blood- stained when granulation tissue is present.
Hearing loss – It is conductive in type and usually moderate to severe, in presence of damage to the ossicles. Sometimes the deafness is very slight when a portion of cholesteatoma might have bridged a gap in the damaged ossicular chain.
Bleeding – From granulation tissue or polypus and may alarm the patients.
Earache– It may be due to sudden reactivation of a quiescent keratoma with inflammation of meatal skin or may indicate a complication.
Dizziness – May be due to serous labyrinthitis either by extension through the windows or by erosion of bony lateral semicircular canal.
Headache – Onset of headache in the presence of CSOM is highly suggestive of intracranial extension of disease.
Otoscopy – Perforation is seen in the pars flaccida or marginally in the posterosuperior part of pars tensa. Cholesteatoma may be visible through the perforation as a greyish paper-like substance or typical pearly sheets of keratin may be recognized. Sometimes a retraction pocket may be seen in the attic and cholesteatoma is seen to invaginate downwards behind an intact tympanic membrane.
AUDIOMETRY
A) Subjective audiometry:
i) Pure tone audiometry.
ii) Bekesy self-recording audiometry.
iii) Speech audiometry
B) Objective audiometry:
i) Impedance audiometry-
Tympanometry
Intra aural reflex measurement
ii) Evoked response audiometry
Pure tone audiometry: An audiometer is an electronic device which produces pure tones, the intensity of which can be increased or decreased in 5dB steps. Usually air conduction thresholds are measured for tones of 125, 250, 500, 1000, 2000, 4000, and 8000 Hz and bone conduction thresholds for 250, 500, 1000, 2000 and 4000 Hz. The amount of intensity that has to be raised above the normal level is a measure of the degree of hearing impairment at that frequency. It is charted in the form a graph called audiogram. The difference in the thresholds of air-bone conduction (A-B gap) is a measure of the degree of conductive deafness. Audiometer is so calibrated that the hearing of a normal person, both for air and bone conduction, is at 0 dB and there is no A-B gap.
When difference between the two ears is 40 dB or above in air conduction thresholds, the better ear is masked to avoid getting a shadow curve from non-test better ear. By pure tone audiometry threshold of hearing by air and bone conduction and thus the degree and type of hearing loss can be measured.
WHO (1980) recommended the following classification on the basis of pure tone audiogram for the degree of hearing loss.
Mild – 26-40 dB
Moderate – 41-55 dB
Moderately severe – 56-70 dB
Severe – 71-90 dB
Profound more than 91 dB
MYRINGOPLASTY
Myringoplasty is the operation specially designed to close tympanic membrane defects. The approach to the ear can be permeatal (transcanal), endaural or postaural.
Approaches:
A permeatal approach has the advantage of least disturbance to the patient but gives limited access and can be difficult in narrow ear canals, which may require drilling of the bone to achieve a satisfactory view. Depending on technique an external incision will usually be needed to harvest graft material.
The endaural incision gives good access to posterior perforations and also to the oval window area. Fascia can be taken through the upper extension of the incision. Anterior perforations can, however be a problem because of lack of access. Bone can be removed from the anterior canal wall but there is a risk of exposure of the temporo-mandibular joint and also of stenosis.
A postaural incision gives excellent anterior access. The posterior view may be slightly restricted but can be improved quite easily by drilling bone away posteriorly from an area already denuded of meatal skin. Fascia is also easily accessible.
GRAFT MATERIALS:
The materials available for grafting are temporalis fascia, connective tissue, perichondrial cartilage or vein. Temporalis fascia is the most commonly employed as it is effective and easily harvested through the same incision and is used to gain access to the ear.
PROCEDURE (Underlay technique) :
This technique is more commonly used in which posterior half of the tympanic membrane is to elevate by dissecting the fibrous annulus out of .its groove in the bone. The graft can then be placed under the tympanic membrane remnant. This considerably, reduces the risk of burying squamous epithelium and provides a more secure location for the graft and virtually eliminates lateralization or blunting.
The placement of the graft in relation to the malleus is a matter of some debate. If placed lateral to the handle the new drum may become lateralized. It is probably wise therefore to place the graft deep to the malleus handle to ensure a proper relationship of graft to malleus.
The graft, epithelial remnants and meatal skin are all carefully repositioned to ensure a correct anatomical alignment. The meatus is then usually packed, but the range of materials used is very wide: various oinments, ribbon gauze impregnated with a range of pharmaceuticals products, sponges and foams, sometimes with protective strips of plastic sheet or oiled silk. The length of time they are left in the ear also varies greatly, from days to weeks. This would all suggest that the packing of the meatus may not be a very important part of the procedure.
This basic technique has numerous variations depending on the site and size of the perforation.
Posterior perforations can be closed by simply raising the posterior half of the drum remnant and sliding the graft underneath. Similarly an inferior perforation can be dealt with using a limited approach. Anterior perforations and subtotal perforations, usually require more extensive elevation. It is wise to carry the dissection of the annulus well forward, superiorly and inferiorly, when performing an underlay graft. This makes positioning much easier later.
Whether remnants need to be dissected off the malleus handle is a matter of opinion, but it needs to be done with care to avoid cochlear trauma. It would, however, appear that the more the tissues are elevated and the wider the grafts bed, the higher the take rate.
In cases in which there is no anterior rim, location of the anterior part of the graft is a problem. An overlay technique taking the dissection up the anterior canal wall provides location but with loss of the angle by blunting. A similar problem sometimes arises if the anterior annulus is raised and the graft tucked underneath. However, a limited tunnel, 1-2mm wide, under the anterior annulus can be used to pull a small tag of graft material through the tunnel and so locate the unstable segment.
There is also disagreement as the need or otherwise to support the graft material in the middle ear. The concern is that graft will collapse at the edge, especially anteriorly.
Many surgeons who use the underlay technique, fill the middle ear with gel foam to support the graft. However, if a good location technique is used with anterior tagging, if necessary, and the patient is encouraged to autoinflate a day or two after surgery, then gel foam does not seem to be necessary.
The use of nitrous oxide during general anaesthesia for myringology is also in question. The concern is that the nitrous oxide diffuses into the middle ear and mastoid across the epithelium and raises the pressure slightly within the tympanomastoid space. Overlay grafts can be dislodged by this pressure and surgeons who use this technique usually try to avoid the use of this anaesthetic agent.
In underlay grafts, especially when the graft is placed deep to the malleus handle, a positive pressure is helpful as it pushes the graft up into contact with the graft bed, making final adjustment to the graft easier and providing a check location.
Results of tympanic membrane repair vary according to technique, but more importantly are affected by the experience of the surgeon. Myringoplasty can be expected to close 90 percent of perforations with a follow-up of 12 months in experienced hands.
PATIENTS AND METHODS
Study place and study period:
This study was carried out in the department of Otolaryngology and Head-Neck Surgery, SirSalimullahMedicalCollege and MitfordHospital, Dhaka, from July 2004 to June 2006.
Sampling method and sampling Size:
Purposive sampling from all consecutive patients of chronic suppurative otitis media (tubotympanic variety) admitted in ENT department of SirSalimullahMedicalCollege and MitfordHospital, Dhaka, during the study period were selected for the study as per the criteria has been described below. A total number of 60 patients were identified accordingly and were included in this study. The Pre and post-operative audiometric evaluation was done for assessment of hearing improvement. Myringoplasty was done by senior surgeons (professor, associate professor and assistant professor) and junior surgeons (registrar and resident surgeon).
Inclusion criteria:
a) Age between 15-45 years.
b) Chronic suppurative otitis media – tubo-tympanic variety with dry perforation (for 3 months) having no other lesions in the external ear, middle ear or inner ear.
c) Pure tone audiogram finding showing mild to moderate hearing loss.
Exclusion criteria:
a) Age below 15 years and above 45 years.
b) Evidence of cholesteatoma or attico-antral disease.
c) Pure tone audiogram finding showing severe to profound hearing loss.
d) Previous tympanic surgery.
e) Traumatic perforation.
f) Tympanosclerosis
g) Previous ossiculoplasty.
Study design:
This was a prospective consecutive and cross-sectional experimental type of study
Measurement of outcome of variables:
(A) Demographic variables:
– Age
– Sex
– Socio-economic status
– Occupation
– Residence
(B) Clinical variables:
– Ear involvement
– Clinical feature
– Size of perforation
– Site of perforation
– Approach of operation
– Hearing status
Data collection:
A predesigned structured questionnaire was made and data was collected using this questionnaire
Ethical clearance:
All the patients were thoroughly explained about the purpose of the study. It was assured that all information gathered is strictly confidential and the procedure will bring no harm nor any extra cost involvement to the patient, rather it will help the doctors for proper diagnosis and management. After detail discussion written informed consents were obtained from the patients.
Study method:
For collection of relevant data two methods were followed – interviewing and filling the observational checklist (questionnaire). Prior to interview, the purpose of the study was elaborated clearly to the respondents asking questions. After taking verbal consent the interview schedule was filled according to response. The findings were recorded in the checklist.
The assessment of the patient was established on the basis of history, clinical examination, pure-tone audiometry, tympanomentry and other relevant investigations.
36 patients were operated under general anaesthesia and the rest 24 patients were operated under local anaesthesia. The incision was given either post auricular or permeatal depending on the size of the external ear canal and the position of the perforation. In all cases underlay technique was applied and temporalis fascia was taken as a graft material.
The patients were post operatively followed up at weekly interval for the first month and fortnightly for the next one month. At the follow-up examination, outcome of myringoplasty was regarded as successful if the ear was dry and the tympanic membrane was mobile and intact. The audiometric tests were performed after two months according to ISO standards (1970). The results were presented as audiological hearing improvement before operation and at the last follow-up examination.
Operational definitions in the study-
Socio-economic groups as per the report of household income and expenditure survey Bangladesh Bureau of statistics, 2005- depending on monthly per capita income:-
Poor class: Upto taka 5000 per month.
Middle class: Taka 5000 -10000 per month.
Upper class: Taka 10000 – and above per month.
The size of the perforations were small perforation – perforations of the tympanic membrane less then 1/4th of its diameter, medium size perforation – perforations of the tympanic membrane between the 1/4th to ½ of its diameter and subtotal perforation – perforations of the tympanic membrane up to 3/4th of its diameter (Sade et al., 1981).
Data analysis:
All collected data were checked and were verified thoroughly to reduce the inconsistency. The numerical data obtained from this study were compiled and analyzed using standard statistical method (Rahim, 2006). For statistical analysis a standard scientific calculator was used. The results are presented here in tables. For statistical evaluation of hearing status `t’ test (paired) was applied.
OBSERVATIONS AND RESULTS:
After collection, the data were analyzed according to the variables for the purpose of the study. For better understanding all data were compiled and tabulated accordingly. The results have been arranged in tabular form. The interpretation of the tables are as follows:
Table-I
Distribution of patients according to age (inclusive) and graft-take rate (n=60)
Age range (years) | No. of patients | Percentage of Patients | No. of graft taken cases | Percentage of graft taken cases |
15-20 | 22 | 36.67 | 19 | 86.36 |
21-30 | 32 | 53.33 | 29 | 90.62 |
31-40 | 4 | 6.67 | 3 | 75.00 |
41-45 | 2 | 3.33 | 1 | 50.00 |
Table-I shows that the age range of patients were from 15 to 45 years with an average age of 24 years. The highest number of patients were in the 21-30 years age group numbering 53.33%. Graft-take rate was also maximum in this age group (90.62%).
Table-II
Distribution of patients according to sex and graft-take rate (n=60)
Sex | No. of patients | Percentage of Patients | No. of graft taken cases | Percentage of graft taken cases |
Male | 34 | 56.67 | 30 | 88.23 |
Female | 26 | 43.33 | 22 | 84.61 |
Table-II shows that the number of male patients was more than those of female. There was no gross difference in the graft-take rate (88.23%) vs (84.61%) in male and female respectively.
Table-III
Socio-economic condition of patients (n = 60)
Socio-economic condition | No. of patients | Percentage |
Poor Class | 4 | 6.67 |
Middle Class | 48 | 80.00 |
Upper Class | 8 | 13.33 |
Table-III shows majority of the patients came from middle class family.
Table-IV
Occupation status of patients (n = 60)
Occupation status | No. of patients | Percentage |
Labourers | 8 | 13.33 |
Farmers | 6 | 10.00 |
Businessmen | 18 | 30.00 |
Housewives | 15 | 25.00 |
Students | 13 | 21.67 |
Table-IV shows that majority of the patients were businessmen, housewives, and students. Among them 30% were businessmen, 25% were housewives 21.67% were students, 13.33% were labourers and the rest 10% were farmers.
Table-V
Residence of the patients (n = 60)
Residence | No. of patients | Percentage |
Rural | 32 | 53.33 |
Urban | 28 | 46.67 |
Table-V shows that majority of the patients came from rural area.
Table-VI
Distribution of patients according to ear involvement and graft-take rate (n =60)
Ear involvement | No. of patients | Percentage of patients | No. of graft taken cases | Percentage of graft taken cases |
Unilateral | 38 | 63.33 | 33 | 86.84 |
Bilateral | 22 | 36.67 | 19 | 86.36 |
Table-VI shows that 38 patients had unilateral and 22 had bilateral perforations (operation was done only in one ear). The success rate was 86.84% in the unilateral and 86.36% in the bilateral cases.
Table-VII
Distribution of patients according to clinical presentation (n =60)
Clinical presentation | No. of patients | Percentage |
H/o intermittent aural discharge (3 months back) | 60 | 100 |
Hearing impairment | 60 | 100 |
Tinnitus | 2 | 3.33 |
Table-VII shows that majority of the patients were presented with intermittent aural discharge and hearing impairment which were the commonest symptoms.
Table-VIII
Distribution of patients according to size of perforation and graft-take rate (n = 60)
Size of perforation | No. of patients | Percentage of patients | No. of graft taken cases | Percentage of graft taken cases |
Small perforation | 8 | 13.33 | 8 | 100 |
Medium size perforation | 37 | 61.67 | 32 | 86.49 |
Sub total perforation | 15 | 25.00 | 12 | 80.00 |
Table-VIII shows that medium size perforations (86.49%) were the commonest in our study. Success rate was more in case of small (100%) and medium size perforations (86.49%) than that of sub-total perforation (80.00%).
Table-IX
Distribution of patients according to site of perforation and graft-take rate (n = 60)
Site of perforation | No. of patients | Percentage of patients | No. of graft taken cases | Percentage of graft taken cases |
Posterior (Behind the umbo) | 6 | 10 | 6 | 100 |
Central (Around the umbo) | 45 | 75 | 36 | 86.67 |
Anterior (In fornt of the umbo) | 9 | 15 | 7 | 77.78 |
Table-IX shows that central perforations were the commonest. Graft-take rate was more common in posterior (100%) than anterior and central perforations.
Table-X
Distribution of patients according to the approach of operation and graft-take rate (n = 60)
Approach of operation | No. of patients | Percentage of patients | No. of graft taken cases | Percentage of graft taken cases |
Post-auricular | 52 | 86.67 | 45 | 86.54 |
Permeatal | 8 | 13.33 | 7 | 87.50 |
Table-X shows that most common approach was post-auricular route (86.67%) followed by permeatal route (13.33%). There was no gross difference in graft-take rate with regard to approach of surgery.
Table-XI
Overall results of operations (n = 60)
Tympanic Membrane | No. of patients | Percentage of patients |
Primary take (intact & mobile tympanic membrane) | 52 | 86.67 |
Graft failure:- | 8 | 13.33 |
(a) Post operative infection | 4 | 6.67 |
(b) Re perforation | 4 | 6.67 |
Table-XII shows that the overall graft-take was 52 (86.67%) and total failure was 8 (13.33%).
Table-XII
Hearing results of operations (n = 60)
A) Hearing status before and after operation (n=60)
No. of Patients | Average pre-operative air conduction threshold | Average post- operative air conduction threshold |
22 | 26.80 dB | 19.10 ** |
32 | 32.40 dB | 20.30 ** |
04 | 34.50 dB | 23.80 ** |
02 | 40.50 dB | 28.70 ** |
** P<0.01 in `t’ test (paired)
B) Overall hearing results:
| Mean dB |
Pre-operative air conduction threshold | 33.55 |
Post-operative air conduction threshold | 22.97 |
Improvement of air conduction threshold | 10.58 |
Table- XIII B shows that pre-operative and post-operative air conduction threshold were 33.55 dB and 22.97 dB respectively with a mean audiological improvement of 10.58dB.
C) Distribution of patients according to hearing improvement or not
Hearing improvement or not | No. of patients | Percentage of patients |
Hearing improvement | 41 | 68.33 |
No hearing improvement | 19 | 31.67 |
Table-XIII C shows that 41 patients had hearing improvement and 19 patients had no hearing improvement.
DISCUSSION:
Chronic suppurative otitis media (CSOM) with or without complications continues to affect a large number of patients particularly in developing countries. The major causes of this problem are negligency and lack of proper medical attention. CSOM of tubo-tympanic variety is very common in our country (Rahim, 2006)
In this study the graft-take rate was 86.67% (52 out of 60) and the graft failure was 13.33 (8 out of 60). The graft-take rate was more than Kotecha et al. (1999) (82%). The cause may be due to the fact that the most of the operations were done by experienced surgeons and there was less infection. The graft-take rate was similar to Fisch (1994) (86%).
In this study, age range of patients were from 15 years to 45 years with a mean age of 24 years. Patients age has generally been considered as an influencing factors for surgical outcome. In this study maximum success rate was found within the age group of 21-30 years (90.62%) followed by 15-20 years (86.31%) and 31-40 years (75.00%) respectively. Similar results were observed by Vrabec et al. (1997).
This is due to low incidence of upper respiratory tract infection and better Eustachian tube function in this age (Vrabec et al., 1997). Our study age group also matches with this facts and findings.
Here the number of male patients are more than those of female. But there was no significant difference in graft-take rate in case of male (88.23%) and female (84.61%). Majority of the patients came from middle class family which was also found by Bhuiyan (2002).
In this study most of the patients of chronic suppurative otits media had unilateral involvement. In the case of bilateral involvement, myringoplasty was done only in one ear in one sitting. Graft-take rate was 86.84% in case of unilateral disease and 86.36% in case of bilateral disease, a difference that was not statistically significant. In Kessler et al. (1994) and Denoyelle et al (1999) study, graft-take rate was higher in unilateral than bilateral disease. The discrepancy between our results and those of Kessler et al. (1994) and Denoyelle et al. (1999) may be due to the fact that some pathological conditions like, chronic tonsillitis, chronic rhino- sinusitis, deviated nasal septum, chronic pharyngitis etc may affect the graft-take rate. In our study, the incidence of these pathological conditions were less.
With regared to the role of size of perforation, medium size perforations were the commonest in our study. Success rate was more in case of small (100%) and medium size perforation (86.49%) than that of subtotal perforations (80%). Similer results were also reported by Sade et al. (1981).
The site of perforation statistically affect outcome in our series as has been previously reported by others (Koch et al., 1990, Podoshin et al., 1996). Central perforations were the commonest. Success rate of posterior perforations (100%) are more than central (86.67%) and anterior perforations (77.78%). Our finding of a higher rate of surgical failure in anterior perforation in comparison to posterior perforation, may be due to the more limited vascularization of the anterior part of the ear drum (Denoyelle et al., 1999) and also due to limited access to this perforation.
Surgical approach depends on dimension of external auditory canal, site of perforations as well as surgerons option. In this study, myringoplasty was done only through postauricular (86.67%) and permeatal (86.50) approaches. No significant difference was found between these two approaches which was also found by Kotecha et al. (1999).
The mean pre-operative air conduction threshold in the study cases were 33.55 dB. While the mean post-operative air-conduction threshold after two months were 22.97 dB with a mean audiological improvement of 10.58 dB. The best improvement was observed within frequency range of 250-1000 Hz. Postopeative hearing was improved in only 41 cases (68.33%) and in 19 cases no hearing improvement was found. This hearing gain was more than Doyle et al. (1972) (52%). The cause may be due to the fact that our cases had least tympanosclerosis, middle ear scarring or graft thickening. No sensori-neural hearing loss was observed after surgery. In some successful cases, hearing was not improved significantly after surgery despite having the tympaninc membrain healed perfectly and the middle ear remain aerated. Sheehy and Anderson (1990) stated that in most cases of CSOM, even though the ossicular chain may appear normal, there is some factors of scar tissue around the ossicular chain that prevents total restoration of hearing.
The overall success rate was 86.67% (52 out of 60). Out of 8 graft failure patients, 4 cases may be due to post-operative infection and 4 cases may be due to reperforations which were caused by some predisposing factors like chronic tonsillitis, chronic rhino-sinusitis, chronic pharyngitis etc. Similar results were reported by Sadel et al. (1981), Sheehy (1984), Cody (1973) and Pahakka et al. (1979). Graft failure occurred during the first 8 weeks. Four cases developed small perforations which were healed by conservative treatment. None of the patients developed epithelial pearl, anterior blunting, medialization or lateralization of graft which was similarly reported by Sade et al. (1981). Crusting and otitis externa were seen in two successful cases those were treated accordingly.
For statistical analysis of preoperative and postoperative hearing threshold, ‘t’ test (paired) was applied. The ‘p’ value of ‘t’ test (paired) was <0.01 which is statistically significant, that means there is a difference between preoperative and postoperative hearing threshold which indicates significant improvement of hearing.
SUMMARY:
A prospective study was carried out from July 2004 to June 2006 at the department of ENT, SSMC, and MitfordHospital, Dhaka with the aims to assess the graft-take rate as well as hearing improvement. This study included 60 patients those underwent myringoplasty operations by underlay technique with temporalis fascia graft.
In this study graft-take rate was 86.67 after 2 months. The age range of patients was 15-45 years. Highest number of patients was in the age group 21-30 years and graft-take rate was also maximum in this age group. Out of 60 patients, male 56.67% and female was 43.33%. There was no gross difference in graft-take in respect with sex.
The surgical success rate was 86.84% in the unilateral and 86.36% in the bilateral cases. Small size (100%) and medium size (86.49%) perforations had more success rate than subtotal perforation (80%). Success rate of posterior perforation (100%) was more than central (86.67%) and anterior perforation (77.78%). Most of the operation was done under general anaesthesia (60%) and the rest (40%) was under local anaesthesia. The success rate was almost similar in postauricular (86.5%) and permeatal approach (87.5%).
The mean preoperative air-conduction threshold in the 60 cases was 33.55 dB, while the mean air-conduction threshold cases was 22.97 dB with a mean audiological improvement of 10.58 dB. 41 cases had hearing improvement while 19 cases had no hearing improvement. No serious complications, such as transient or permanent facial nerve paralysis or severe sensorineural hearing loss were noted.
CONCLUSION:
From this study it can be concluded that myringoplasty is a valid treatment modality for closing the perforation of tympanic membrane, prevention of infection and improvement of hearing in CSOM (tubo-tympanic variety). As the surgical outcome depends on the status of middle ear (dry or wet) it is essential that the preoperative inflammatory changes in the middle ear mucosa should be carefully evaluated and its appropriate medical treatment should be considered. It is also evident that good audiological result in successful cases are associated with a high probable return to normal function and lifestyle at any age.