A three-member Albert Einstein College of Medicine research team made a discovery that may improve the success of stem-cell transplants, which are routinely utilized for patients with cancer, blood problems, or autoimmune illnesses caused by faulty stem cells that produce all of the body’s blood cells. The findings from mice were published today in the journal Science.
“Our research has the potential to improve the success of stem-cell transplants and expand their use,” explained Ulrich Steidl, M.D., Ph.D., professor and chair of cell biology, interim director of the Ruth L. and David S. Gottesman Institute for Stem Cell Research and Regenerative Medicine, and the Edward P. Evans Endowed Professor for Myelodysplastic Syndromes at Einstein, and deputy director of the National Cancer Institute-designated Montefiore Einstein Comprehensive Cancer Center (MECCC).
Dr. Steidl, Einstein’s Britta Will, Ph.D., and Xin Gao, Ph.D., a former Einstein postdoctoral fellow, now at the University of Wisconsin in Madison, are co-corresponding authors on the paper.
Trogocytosis plays a role in regulating immune responses and other cellular systems, but this is the first time anyone has seen stem cells engage in the process. We are still seeking the exact mechanism for how HSCs regulate trogocytosis.
Dr. Gao
Mobilizing Stem Cells
Stem-cell transplants are used to treat conditions in which an individual’s hematopoietic (blood-forming) stem cells (HSCs) have become malignant (as in leukemia or myelodysplastic syndromes) or insufficient (as in bone marrow failure and severe autoimmune disorders). The therapy includes injecting healthy HSCs from donors into patients. To collect those HSCs, donors are administered a medication that causes HSCs to mobilize, or escape, from their natural homes in the bone marrow and enter the bloodstream, where they can be isolated from other blood cells and transplanted. However, medicines used to mobilize HSCs frequently do not liberate enough of them for the transplant to be successful.
“It’s normal for a tiny fraction of HSCs to exit the bone marrow and enter the bloodstream, but what controls this mobilization isn’t well understood,” said Dr. Will, associate professor of oncology and of medicine, and the Diane and Arthur B. Belfer Faculty Scholar in Cancer Research at Einstein, and the co-leader of the Stem Cell and Cancer Biology research program at MECCC. “Our research represents a fundamental advance in our understanding, and points to a new way to improve HSC mobilization for clinical use.”
Tracking Trogocytosis
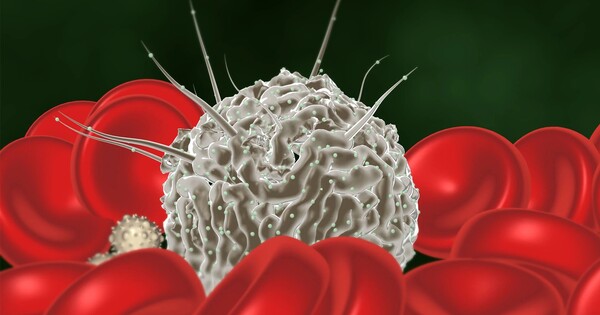
The researchers suspected that variations in proteins on the surface of HSCs might influence their propensity to exit the bone marrow. In studies involving HSCs isolated from mice, they observed that a large subset of HSCs display surface proteins normally associated with macrophages, a type of immune cell. Moreover, HSCs with these surface proteins largely stayed in the bone marrow, while those without the markers readily exited the marrow when drugs for boosting HSCs mobilization were given.
After combining HSCs with macrophages, the researchers noticed that certain HSCs engaged in trogocytosis, a process in which one cell type removes membrane components from another and incorporates them into their own membranes. HSCs with high quantities of the protein c-Kit on their surface were able to undergo trogocytosis, leading their membranes to be enhanced with macrophage proteins and making them considerably more likely than other HSCs to remain in the bone marrow. The findings indicate that inhibiting c-Kit might impede trogocytosis, resulting in more HSCs being mobilized and ready for transplantation.
“Trogocytosis plays a role in regulating immune responses and other cellular systems, but this is the first time anyone has seen stem cells engage in the process. We are still seeking the exact mechanism for how HSCs regulate trogocytosis,” said Dr. Gao, assistant professor of pathology and laboratory medicine at the University of Wisconsin-Madison, Madison, WI.
The researchers intend to continue their investigation into this process: “Our ongoing efforts will look for other functions of trogocytosis in HSCs, including potential roles in blood regeneration, eliminating defective stem cells and in hematologic malignancies,” added Dr. Will.