An important protein that serves as a checkpoint for calcium entering cells increases the development of oral cancer and causes pain, according to a recent study led by researchers from the NYU College of Dentistry and published in Science Signaling.
Oral cancer generates chronic discomfort that worsens as it spreads, therefore targeting the ORAI1 calcium channel protein may offer a fresh method of treatment.
“Our results show that the ORAI1 channel fuels the growth of oral cancer tumors and produces an abundance of molecules that, once secreted, interact with neurons resulting in an increased sensitivity to pain,” said Ga-Yeon Son, a postdoctoral fellow in the Department of Molecular Pathobiology at NYU College of Dentistry and the study’s first author.
The keepers of the gates of heaven
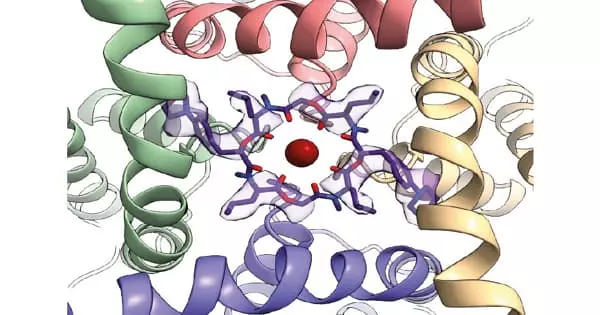
The amount of calcium that enters cells is heavily regulated by ORAI calcium channels, which get their name from the three sisters who guarded the gates of heaven on Mount Olympus in Greek mythology.
“These calcium channels can be a source of good or bad for cells,” said Rodrigo Lacruz, professor of molecular pathobiology at NYU College of Dentistry and the study’s senior author. “Calcium entering cells is necessary for many good things, but too much calcium for a long time has the opposite effect.”
Few research have examined the role of ORAI1 in cancer and pain, despite the fact that calcium channels have been associated to several malignancies, including cancer development.
“Calcium influx through ORAI1 channels has been well known to contribute to the regulation of gene expression by activating gene transcription factors in the cells. Notably, our investigation extends its function in regulating gene expression to altering oral cancer pain,” said Son.
Less ORAI1, less cancer growth and pain
The scientists initially examined tissue samples taken from healthy tongues and malignancies from human oral cancer. The ORAI1 gene, which encodes for the ORAI1 calcium channel, was discovered to be highly overexpressed in the tumors but not in healthy tissue.
Our results show that the ORAI1 channel fuels the growth of oral cancer tumors and produces an abundance of molecules that, once secreted, interact with neurons resulting in an increased sensitivity to pain.
Ga-Yeon Son
They then examined human oral cancer cells and found that activating the ORAI1 calcium channel (but not other calcium channels) caused a large influx of calcium into cancer cells. A calcium-dependent enzyme termed matrix metalloprotease 1 (MMP1), which is released outside of cancer cells, increased as a result of this influx. MMP1 is widely expressed in a variety of cancers, including oral cancer, where it is linked to metastasis and a bad prognosis.
Removing the ORAI1 gene from oral cancer cells changed the course of the disease in animal studies. When mice were inoculated with cancer cells lacking the ORAI1 gene, tumors grew more slowly and were less painful.
“These findings demonstrate an important role for ORAI1 in oral cancer progression and pain, but what is the mechanism? We wondered if MMP1 could be the messenger relaying pain,” said Lacruz.
In collaboration with NYU Pain Research Center scientists Rajesh Khanna and Yi Ye, the team looked at the levels of MMP1 expressed in the fluid surrounding oral cancer cells and saw that cells lacking the ORAI1 gene secreted less MMP1 into the surrounding fluid. The trigeminal ganglia are a group of facial nerves that transmit pain in oral cancer. They blended the fluid with neurons from these nerves.
The fluid from cancer cells lacking the ORAI1 gene did not cause the neurons to react strongly, whereas the MMP1-rich fluid from cancer cells with the ORAI1 gene caused a rise in action potentials, which is a requirement for the transmission of pain.
“This gives us evidence that an abundance of MMP1 may generate increased sensitivity to pain,” said Lacruz.
The researchers also ran experiments with abnormal but non-cancerous cells. These non-invasive cells become invasive when the ORAI1 gene was overexpressed, suggesting that ORAI1 may be involved in the transformation of non-malignant cells into cancerous ones.
Future research: blocking ORAI
Several FDA-approved drugs block the ORAI1 calcium channel, but they have not yet been tested in oral cancer. Future research will examine if an ORAI-blocking medicine can be accurately administered into animal models’ tongues using nanoparticles to halt the spread and discomfort of oral cancer.
“In light of the ongoing opioid crisis, our study paves the way for validating novel pain treatments in oral cancer,” said Rajesh Khanna, director of the NYU Pain Research Center, professor of molecular pathobiology at NYU Dentistry, and a co-author of the study.
“Ultimately, our hope is that targeting the ORAI1 channel in oral cancer can prevent or delay the progression from oral epithelial dysplasia to oral cancer tumors and concurrently alleviate the pain burden experienced by oral cancer patients,” added Son.
Additional study authors include Nguyen Huu Tu, Maria Daniela Santi, Santiago Loya Lopez, and Guilherme H. Souza Bomfim of NYU College of Dentistry; Manikandan Vinu, Ariya Chaloemtoem, Rama Alhariri, and Youssef Idaghdour of NYU Abu Dhabi; and Fang Zhou of NYU Langone Health.